Nelson de Araujo Vega, Hugo Alejandro Vega Ortega, Alfio José Tincani, Ivan Felizardo Contrera Toro
ABSTRACT
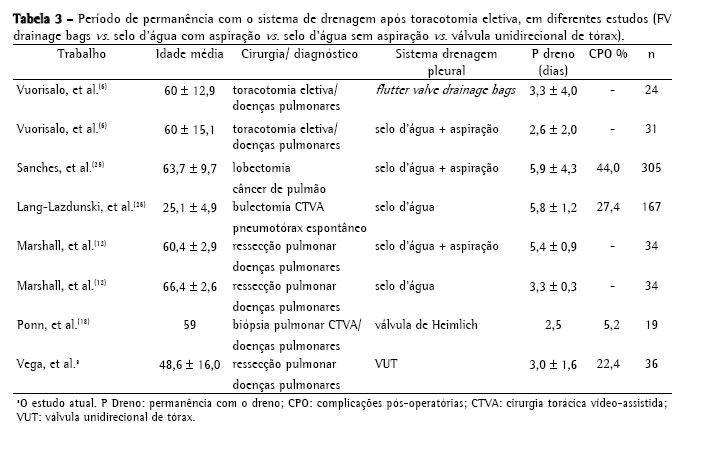
Objective: To evaluate pleural drainage using a one-way flutter valve following elective lung resection. Methods: This was a prospective study, with descriptive analysis, of 39 lung resections performed using a one-way flutter valve to achieve pleural drainage during the postoperative period. Patients less than 12 years of age were excluded, as were those submitted to pneumonectomy or emergency surgery, those who were considered lost to follow-up and those in whom water-seal drainage was used as the initial method of pleural drainage. Lung expansion, duration of the drainage, hospital stay and postoperative complications were noted. Results: A total of 36 patients were included and analyzed in this study. The mean duration of pleural drainage was 3.0 ± 1.6 days. At 30 days after the surgical procedure, chest X-ray results were considered normal for 34 patients (95.2%). Postoperative complications occurred in 8 patients (22.4%) and were related to the drainage system in 3 (8.4%) of those. Conclusions: The use of a one-way flutter valve following elective lung resection was effective, was well tolerated and presented a low rate of complications.
Keywords: Drainage; Postoperative complications; Thoracic surgery.
RESUMO
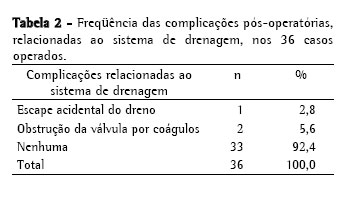
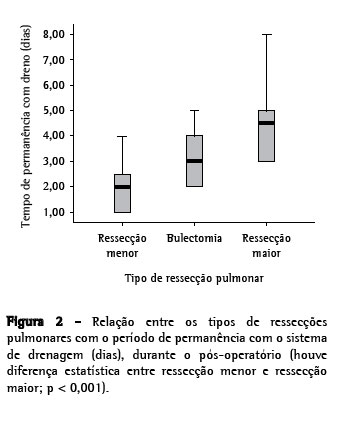
Objetivo: Avaliar a drenagem pleural através de válvula unidirecional de tórax no pós-operatório de ressecção pulmonar eletiva. Métodos: Foram realizadas 39 ressecções pulmonares, de forma prospectiva e com análise descritiva, em pacientes que utilizaram a válvula unidirecional de tórax (VUT) como o método de drenagem pleural durante o período pós-operatório. Foram excluídos os pacientes com idade inferior a 12 anos, os submetidos à pneumectomia ou a operação de urgência, os que não completaram o seguimento do estudo e os pacientes que utilizaram o sistema de frasco em selo d'água como método inicial de drenagem pleural. Observou-se a expansão pulmonar, o tempo de permanência com o sistema de drenagem, o período de internação e as complicações pós-operatórias. Resultados: Neste estudo, foram incluídos e analisados 36 pacientes. A média de permanência com o sistema de drenagem pleural foi de 3,0 ± 1,6 dias. O laudo da radiografia de tórax, realizado após 30 dias do procedimento cirúrgico foi considerado normal em 34 (95,2%) pacientes. Ocorreram oito (22,4%) casos de complicações pós-operatórias, sendo três (8,4%) relacionadas à VUT. Conclusões: A utilização da VUT no pós-operatório de ressecção pulmonar eletiva foi eficiente, bem tolerada e apresentou baixo índice de complicação.
Palavras-chave: Drenagem; Complicações pós-operatórias; Cirurgia torácica.
Introdução