ABSTRACT
Mechanical ventilation can be a life-saving intervention, but its implementation requires a multidisciplinary approach, with an understanding of its indications and contraindications due to the potential for complications. The management of mechanical ventilation should be part of the curricula during clinical training; however, trainees and practicing professionals frequently report low confidence in managing mechanical ventilation, often seeking additional sources of knowledge. Review articles, consensus statements and clinical practice guidelines have become important sources of guidance in mechanical ventilation, and although clinical practice guidelines offer rigorously developed recommendations, they take a long time to develop and can address only a limited number of clinical questions. The Associação de Medicina Intensiva Brasileira and the Sociedade Brasileira de Pneumologia e Tisiologia sponsored the development of a joint statement addressing all aspects of mechanical ventilation, which was divided into 38 topics. Seventy-five experts from all regions of Brazil worked in pairs to perform scoping reviews, searching for publications on their specific topic of mechanical ventilation in the last 20 years in the highest impact factor journals in the areas of intensive care, pulmonology, and anesthesiology. Each pair produced suggestions and considerations on their topics, which were presented to the entire group in a plenary session for modification when necessary and approval. The result was a comprehensive document encompassing all aspects of mechanical ventilation to provide guidance at the bedside. In this article, we report the methodology used to produce the document and highlight the most important suggestions and considerations of the document, which has been made available to the public in Portuguese.
Keywords:
Respiration, artificial; Practice guidelines as topic; Noninvasive ventilation; Ventilator weaning; Intensive care units
RESUMO
A ventilação mecânica é uma intervenção que pode salvar vidas, mas sua implementação requer uma abordagem multidisciplinar, com a compreensão de suas indicações e contraindicações devido a possíveis complicações. O manejo da ventilação mecânica deveria fazer parte dos currículos durante o estágio clínico; no entanto, os residentes e profissionais em exercício frequentemente relatam pouca confiança no manejo da ventilação mecânica, buscando, muitas vezes, fontes de conhecimento complementares. Artigos de revisão, declarações de consenso e diretrizes de prática clínica tornaram-se importantes fontes de orientação sobre ventilação mecânica e, embora as diretrizes de prática clínica ofereçam recomendações rigorosamente elaboradas, elas levam muito tempo para serem implementadas e podem abordar apenas um número limitado de questões clínicas. A Associação de Medicina Intensiva Brasileira e a Sociedade Brasileira de Pneumologia e Tisiologia patrocinaram a elaboração de um conjunto de orientações abordando todos os aspectos da ventilação mecânica, dividida em 38 tópicos. Ao todo, 75 especialistas de todas as regiões do Brasil trabalharam em duplas para realizar revisões de escopo, buscando publicações sobre seu tópico específico de ventilação mecânica nos últimos 20 anos nas revistas de maior Fator de Impacto nas áreas de terapia intensiva, pneumologia e anestesiologia. Cada dupla produziu sugestões e considerações sobre seus tópicos, apresentados a todo o grupo em uma sessão plenária para modificação, quando necessário, e aprovação. O resultado foi um documento abrangente que engloba todos os aspectos da ventilação mecânica para fornecer orientação à beira do leito. Neste artigo, relatamos a metodologia utilizada para produzir o documento e destacamos as sugestões e as considerações mais importantes do documento, o qual foi divulgado publicamente em português.
Palavras-chave:
Respiração artificial; Guidelines como tópico; Ventilação não invasiva; Desmame do ventilador; Unidades de terapia intensiva
INTRODUCTION Invasive and noninvasive mechanical ventilation (MV) is essential in the treatment of patients with acute respiratory failure and is the most frequently implemented support measure in intensive care units (ICUs).(1,2) Although it is a life-saving measure, MV requires an understanding of its indications, contraindications, and management, as it can be associated with complications, especially when it is implemented inappropriately.(3) Because it is used mainly in severe or potentially severe patients, it involves complex coordination between healthcare providers, including respiratory therapists, nurses, physicians, and other specialists, to ensure optimal patient care, proper ventilator management and timely interventions to avoid complications.
The management of MV is a core competency in critical care training and should be part of the undergraduate curricula in medicine, nursing and physiotherapy, as well as residency and subspecialization in critical care.(4) However, trainees and practicing professionals often report low confidence in managing MV patients and performing basic adjustments(5,6) and seek other sources of knowledge about MV. Since the 1990s, review articles and consensus statements on MV have become important sources of guidance for clinicians.(7) In recent years, most consensuses have employed the Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology(8) to establish clinical practice guidelines.(9-11) This methodology is accepted as the best strategy for providing recommendations based on evidence, but because extensive work is needed to formulate recommendations based on a limited number of clinical questions, it may not be suitable if the intention is to provide a comprehensive document encompassing all aspects of a broad topic, such as MV.
In 2013, the Associação de Medicina Intensiva Brasileira (AMIB) and the Sociedade Brasileira de Pneumologia e Tisiologia (SBPT) published the Brazilian Recommendations for Mechanical Ventilation. (12,13) Twenty-nine topics related to MV and suggestions for MV management were given for most clinical situations. Although a systematic methodology such as the GRADE was not adopted, the document became an important source of guidance for clinicians in Brazil. It was published as a research article in two parts and as a manual in PDF, which could be consulted at the bedside. Since then, new studies have been conducted and published, as well as guidelines on different aspects of ventilatory support, coordinated by different medical societies.(9-11,14-16) In addition, during the coronavirus disease 2019 (COVID-19) pandemic, when many patients required MV, the complexity of the conditions that require ventilatory support and the need for capacity building among healthcare professionals became clear.(17)
As a result, in 2023, AMIB and SBPT sponsored a project to update the recommendations. In this article, we report the methodology used to produce the document and highlight the most important suggestions and considerations of the document, which has been made available to the public (https://indd.adobe.com/ view/017f739a-847f-4587-9bef-15b9c01756ba).
METHODOLOGY The Organizing Committee selected 38 topics related to MV for patients with respiratory failure and other indications of MV that were addressed in this document. Each society indicated members who were considered experts in the field and involved in research and/or teaching of MV in Brazil to be invited to participate in the project. After a formal invitation and confirmation of those who were able to participate in the project, the group of experts was confirmed with 75 participants. The experts were all health care professionals specializing in intensive care, including physicians, nurses, physiotherapists, speech therapists, dentists, and nutritionists. They predominantly worked in the Southeast Region of Brazil (67%), with another 17% from the South Region, 10% from the Northeast Region, 5% from the Central West Region and 1% from the North Region. The participants were divided to work in pairs, and each topic was assigned to a pair of experts. The content to be addressed by each pair in their respective theme was previously determined by the organizing committee at the time of the invitation. Expertise and previous experience with their theme were taken into account when inviting each pair.
The pairs searched PubMed and the Cochrane Central Register of Controlled Trials databases for articles published on the topic. The search was limited to the last twenty years and focused on, but was not limited to, journals in the following areas: Intensive Care, Pulmonology, and Anesthesiology, including the journals of the respective Brazilian societies in these specialties: Critical Care Science (formerly the Revista Brasileira de Medicina Intensiva), the Jornal Brasileiro de Pneumologia, and the Revista Brasileira de Anestesiologia. Based on the results, each pair produced a text relevant to their topic and sent it to the organizing committee, with their respective bibliographic references. The format adopted to provide guidance was as follows: Comment (brief explanation of the topic to be addressed), followed by suggestions and considerations, as defined in table 1.

In addition, we used “Suggestion” for statements based on documents developed by national and international health authorities, such as the World Health Organization or Ministry of Health, and for statements based on well-established medical society guidelines, such as the Advanced Cardiovascular Life Support (ACLS) guidelines. The content prepared by each pair was then compiled and summarized by the Organizing Committee, which prepared all the topics for the pairs to present at a face-to-face meeting held on November 20 and 21, 2023, in Florianópolis, Santa Catarina, Brazil, prior to the Brazilian Congress of Intensive Care Medicine. During the meeting, all pairs presented their suggestions and considerations, submitting them to the evaluation and appreciation of all those present. The plenary held its manifestations freely, and all the suggestions were discussed. When there was no consensus and two alternatives for formulating suggestions/considerations remained after ample discussion, the two alternatives were presented for electronic voting using an anonymous system.
At the end of this stage, the organizing committee compiled the text sent by all the pairs and made the agreed-upon adjustments after the plenary session. The revised document was sent to each expert for review or final adjustments. Finally, the organizing committee reviewed the final edition of the unified document with all the themes.
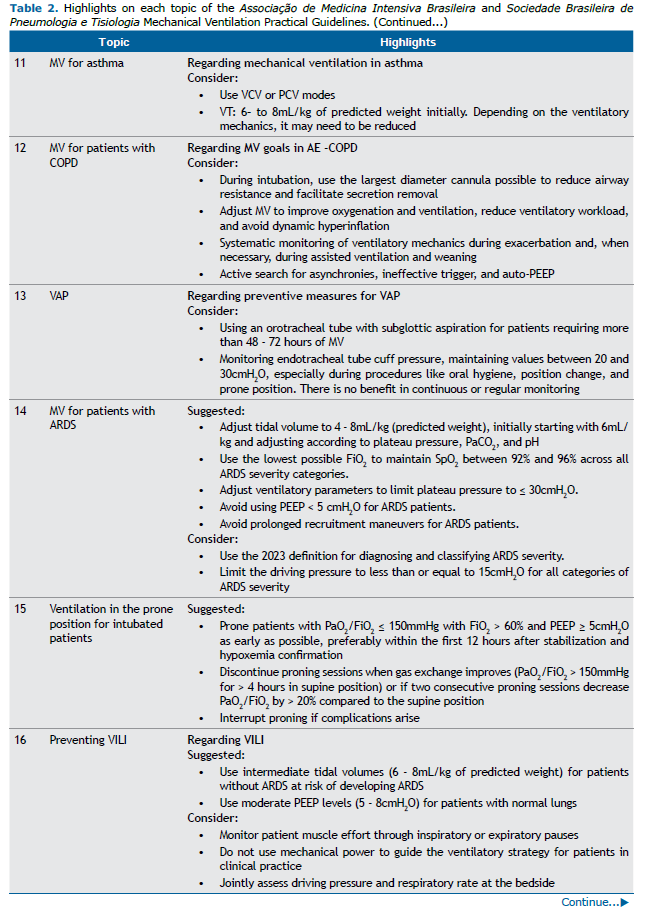
The document included multidisciplinary topics, such as nursing, physiotherapy, nutrition, speech therapy, and dentistry. New topics were added, such as ventilation-induced lung injury (VILI), extracorporeal membrane oxygenation (ECMO), MV in pregnant women, MV in the transport of patients, ICU-acquired weakness, MV in palliative care patients and a specific topic for prone positioning. Table 2 shows the list of topics covered in the document and the most relevant suggestions and considerations for each topic.
COMMENTS The experts made a total of 100 suggestions and 288 considerations in relation to the 38 themes (Figure 1). Consensus with a simple majority was reached during the plenary session for almost all suggestions/considerations, and electronic voting was required for four of the most controversial issues. Table 2 shows the most relevant suggestions and considerations for each topic and the four topics that required discussion. To access all the suggestions and considerations, please refer to the original document, which is freely available on the two societies’ websites (https://indd.adobe.com/ view/017f739a-847f-4587-9bef-15b9c01756ba).
FINAL COMMENTS The development of a practical bedside document and the updating of the previous Brazilian recommendations for mechanical ventilation led to a collaborative effort between AMIB and SBPT. The experts reviewed the latest evidence related to the care of patients undergoing MV, following the proposed methodology. This process generated suggestions and considerations, which were initially discussed and voted on in a plenary meeting and then reviewed by the organizing committee before being published. This document has been made publicly available and is being disseminated by both professional societies to provide guidance at the bedside across the country.
Clinical practice guidelines are considered valuable instruments for narrowing the gap between research findings and actual clinical practice.(18-20) These tools enhance and standardize treatment, optimize patient care, and potentially reduce mortality rates and healthcare costs.(21-23) but are still underutilized in clinical settings.(24) Additionally, there is a need for locally developed clinical guidelines and treatment protocols in low- and middle-income countries (LMICs), as resource limitations may prevent the application of guidelines developed in high-resource settings.(25) Simply translating guidelines and treatment protocols produced in high-resource settings is not enough, as the context in which they are applied is different.
The development of this bedside guide can help fill that gap. Providing guidance on a series of topics related to MV addresses an unmet need in an area with a high burden of disease.(26,27) A large observation study performed in 2013 in several Brazilian ICUs revealed that the mortality of patients under MV was higher than that in high income countries.(26) During the COVID-19 pandemic, the strain imposed on an already overstressed healthcare system led to extremely high mortality in patients who required MV in Brazil.(17,28-30) Although worse outcomes have been reported across the globe, considerable variation has been reported, showing that some ICUs are more resilient and are able to adapt and respond to strain with less impact on patient outcomes.(31) Among many components, a resilient ICU invests in the implementation of evidence- based practices and staff training. For example, the use of protective ventilatory strategies(28) and timely use of noninvasive ventilation(29) are associated with lower mortality, suggesting that the implementation of evidence-based strategies in MV has an impact on patient outcomes, especially in situations of strain.
We produced a comprehensive document addressing 38 topics related to ventilatory support. In almost three quarters of the cases, there were no randomized controlled trials to inform suggestions; therefore, the guidance to readers was less emphatic, with a consideration to use or not use a given intervention. Although the lack of robust evidence prevented us from providing more assertive suggestions on these topics, we believe that the considerations are valuable because evidence in the form of clinical trials is lacking for important topics such as choosing the mode of ventilation or how to adjust the initial settings of a ventilator, which are typically not addressed in clinical practice guidelines produced with methodologies such as GRADE. In the case of specific ventilatory strategies, such as prone positioning, recruitment maneuvers and the use of neuromuscular blockage, more than one randomized controlled trial was available, and a suggestion could be made. Notably, these topics are already covered by two recent clinical practice guidelines and recommendations in the same lines as our suggestions were made.(9,10)
If a lack of training, resulting in low confidence in managing patients under MV among clinicians,(5,6) a lack of adoption of evidence-based strategies in MV(1) and a lack of treatment protocols(32,33) to facilitate the implementation of such strategies contribute to the greater burden of acute respiratory failure in LMICs, these gaps offer a significant opportunity for improvement in outcomes. The dissemination of evidence-based best practices in the form of accessible documents can offer guidance to clinicians at the bedside and inform treatment protocol development. Although the joint statement produced by AMIB and SBPT alone is not sufficient, emphasizing the urgent need for health care capacity building, specialization and training, investments in infrastructure, and other measures to improve healthcare systems and processes of care, it is an important first step.
Despite having been developed to meet the needs of the Brazilian critical care context, two major barriers remain. First, ensuring ample dissemination and consistent adoption.(34) Healthcare professionals’ negative attitudes and beliefs, limited integration of guideline recommendations into organizational structures, time and resource constraints and organizational- and system-level changes are identified barriers.(24) Second, inequalities in ICU resources across Brazil will impact the applicability of some of the suggestions and considerations made in the document. For example, we suggest that high-flow nasal cannulas can be used in a variety of scenarios because randomized controlled trials have shown that they are effective for avoiding intubation and reducing mortality in patients with respiratory failure, but many ICUs in Brazil do not have that technology readily available. The same can be said about the recommendation to use ECMO for refractory hypoxemia and expensive monitoring devices, such as end-tidal CO2 and indirect calorimetry. When preparing suggestions and considerations, we aimed to balance the availability of evidence in favor of such interventions and the Brazilian context, recognizing that although many ICUs in Brazil may not have access to interventions that include complex and/or expensive technology, when the evidence is strong in favor of the benefit they offer, it would not be appropriate to refrain from suggesting their use. On the contrary, we believe that the suggestion for use of evidence-based interventions stated in a document endorsed by two respected medical societies can help inform public health policy in Brazil, supporting the incorporation of technologies that have been shown to reduce mortality, such as noninvasive ventilation, high-flow nasal cannulas(29) and ECMO.(35)
The present study has several limitations: the methodology adopted did not include performing systematic reviews and meta-analyses to make recommendations, as is the case with the GRADE methodology, because with so many topics, it would be impractical to adopt this strategy. In addition, we did not formally evaluate the quality of the studies, as the GRADE methodology typically does to formulate recommendations. The experts were instructed to use their own judgment when selecting references. As a result, it is possible that some of the studies used in the document were at high risk of bias. Therefore, no recommendations were made, and we used a different terminology, with suggestions and considerations. The decision to perform a focused review of each theme, instead of systematic reviews and meta-analyses with PICO questions, was made to allow the document to be as comprehensive as possible. The topics and their scopes were determined by the coordinators by informal consensus and were therefore subject to selection bias. In addition, some topics in the document were not examined in clinical trials; therefore, the considerations made about them were based on physiological studies or expert opinions. The document also has strengths: the topics were thoroughly evaluated by professionals recognized as experts in MV, and there was a plenary discussion of all the topics and voting, when necessary, highlighting the robustness of the suggestions and considerations formulated.
CONCLUSION Evidence-based and up-to-date guidance is essential to ensure that healthcare providers are informed by best practices for the management of patients undergoing mechanical ventilation. This joint statement aims to standardize care, reduce variability in clinical practice, improve patient outcomes, and support teaching in MV. Its implementation can lead to a decrease in complications associated with MV, optimization of the use of resources, and improvement in the quality of patient care.
ACKNOWLEDGMENTS The authors would like to thank Associação de Medicina Intensiva Brasileira (AMIB) and Sociedade Brasileira de Pneumologia e Tisiologia (SBPT) for their support in producing this document. They also thank Magnamed and Medtronic for supporting the Mechanical Ventilation Practical Suggestions and Considerations project.
FUNDING Associação de Medicina Intensiva Brasileira (AMIB) and Sociedade Brasileira de Pneumologia e Tisiologia (SBPT); Magnamed and Medtronic provided unrestricted grants for the development of the Mechanical Ventilation Practical Suggestions and Considerations. However, they were not involved in selecting experts or topics, formulating suggestions and considerations, or writing the manuscript.
AUTHORS’ CONTRIBUTIONS J. C. Ferreira, A. O. A. Vianna, B. V. Pinheiro, I. S. Maia, S. V. Baldisserotto and A. M. Isola participated in the study conception, coordinated the work to develop the suggestions and considerations and interpreted the results; J. C. Ferreira and A. M. Isola wrote the first draft;
A. O. A. Vianna, B. V. Pinheiro, I. S. Maia and S. V. Baldisserotto revised and edited the manuscript versions. All authors approved the final version of the manuscript. The collaborator authors developed the suggestions and considerations, participated in plenary sessions and approved the final version of the full document.
PUBLISHER’S NOTE Conflicts of interest: None.
This article has been co-published with permission in Critical Care Science 2025;37:e20250242en. DOI: https://doi.org/10.62675/2965-2774.20250242-en COLLABORATING AUTHORSAlexandre Biasi Cavalcanti
Instituto de Pesquisa, HCor-Hospital do Coração - São Paulo (SP), Brazil.
Ana Maria Casati Nogueira da Gama
Hospital Universitário “Cassiano Antônio de Moraes”, Universidade Federal do Espírito Santo - Vitória (ES), Brazil.
Angelo Roncalli Miranda Rocha
Hospital Geral do Estado de Alagoas - Maceió (AL), Brazil.
Antonio Gonçalves de Oliveira
Complexo Hospitalar Unimed Recife - Recife (PE), Brazil.
Ary Serpa-Neto
Australian and New Zealand Intensive Care Research Centre, Monash University - Melbourne, Victoria, Australia.
Augusto Manoel de Carvalho Farias
Hospital Português - Salvador (BA), Brazil.
Bianca Rodrigues Orlando
Hospital Escola, Universidade Federal de Pelotas - Pelotas (RS), Brazil.
Bruno da Costa Esteves
Hospital Evangélico de Sorocaba - Sorocaba (SP), Brazil.
Bruno Franco Mazza
Hospital Israelita Albert Einstein - São Paulo (SP), Brazil.
Camila de Freitas Martins Soares Silveira
Hospital Israelita Albert Einstein Goiânia - Goiânia (GO), Brazil.
Carlos Roberto Ribeiro de Carvalho
Instituto do Coração, Hospital das Clínicas, Faculdade de Medicina, Universidade de
São Paulo - São Paulo (SP), Brazil.
Carlos Toufen Junior
Instituto do Coração, Hospital das Clínicas, Faculdade de Medicina, Universidade de
São Paulo - São Paulo (SP), Brazil.
Carmen Silvia Valente Barbas
Instituto do Coração, Hospital das Clínicas, Faculdade de Medicina, Universidade de
São Paulo - São Paulo (SP), Brazil.
Cassiano Teixeira
Universidade Federal de Ciências da Saúde de Porto Alegre - Porto Alegre (RS), Brazil.
Débora Dutra da Silveira
Universidade Federal de São Paulo - São Paulo (SP), Brazil.
Denise Machado Medeiros
Instituto Nacional de Infectologia “Evandro Chagas”, Fundação “Oswaldo Cruz” - Rio de Janeiro (RJ), Brazil.
Edino Parolo
Hospital de Clínicas de Porto Alegre, Universidade Federal do Rio Grande do Sul - Porto Alegre (RS), Brazil.
Eduardo Leite Vieira Costa
Instituto do Coração, Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo - São Paulo (SP), Brazil.
Eliana Bernadete Caser
Hospital Universitário “Cassiano Antônio de Moraes”, Universidade Federal do Espírito Santo - Vitória (ES), Brazil.
Ellen Pierre de Oliveira
Instituto do Coração, Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo - São Paulo (SP), Brazil.
Eric Grieger Banholzer
Pontifícia Universidade Católica do Paraná - Curitiba (PR), Brazil.
Erich Vidal Carvalho
Hospital Universitário, Universidade Federal de Juiz de Fora - Juiz de Fora (MG), Brazil.
Fabio Ferreira Amorim
Escola Superior de Ciências da Saúde, Universidade do Distrito Federal - Brasília (DF), Brazil.
Felipe Saddy
Hospital Pró-Cardíaco - Rio de Janeiro (RJ), Brazil.
Fernanda Alves Ferreira Gonçalves
Hospital das Clínicas, Universidade Federal de Goiás - Goiânia (GO), Brazil.
Filomena Regina Barbosa Gomes Galas
Instituto do Coração, Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo - São Paulo (SP), Brazil.
Giovanna Carolina Gardini Zanatta
Hospital Alvorada - São Paulo (SP), Brazil.
Gisele Sampaio Silva
Universidade Federal de São Paulo - São Paulo (SP), Brazil.
Glauco Adrieno Westphal
Centro Hospitalar Unimed - Joinville (SC), Brazil.
Gustavo Faissol Janot de Matos
Hospital Israelita Albert Einstein - São Paulo (SP), Brazil.
João Claudio Emmerich de Souza
Hospital Federal dos Servidores do Estado - Rio de Janeiro (RJ), Brazil.
João Manoel Silva Junior
Faculdade de Medicina, Universidade de São Paulo - São Paulo (SP), Brazil.
Jorge Luis dos Santos Valiatti
Curso de Medicina, Centro Universitário Padre Albino - Catanduva (SP), Brazil.
José Ribamar do Nascimento Junior
Instituto de Gerenciamento em Fonoaudiologia e Deglutição - São Paulo (SP), Brazil.
José Rodolfo Rocco
Universidade Federal do Rio de Janeiro - Rio de Janeiro (RJ), Brazil.
Ludhmila Abrahão Hajjar
Faculdade de Medicina, Universidade de São Paulo - São Paulo (SP), Brazil.
Luiz Alberto Forgiarini Junior
Universidade Católica de Pelotas - Pelotas (RS), Brazil.
Luiz Marcelo Sá Malbuisson
Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo - São Paulo (SP), Brazil.
Marcelo Alcântara Holanda
Universidade Federal do Ceará - Fortaleza (CE), Brazil.
Marcelo Britto Passos Amato
Instituto do Coração, Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo - São Paulo (SP), Brazil.
Marcelo Park
Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo - São Paulo (SP), Brazil.
Marco Antônio da Rosa e Oliveira
Departamento de Educação Continuada, Imed Group - São Paulo (SP), Brazil.
Marco Antônio Soares Reis
Hospital Madre Teresa - Belo Horizonte (MG), Brazil.
Marcos Soares Tavares
Hospital 9 de Julho - São Paulo (SP), Brazil.
Mario Henrique Dutra de Souza
Hospital Alvorada - Rio de Janeiro (RJ), Brazil.
Marta Cristina Pauleti Damasceno
Santa Casa de Misericórdia de São João da Boa Vista - São Paulo (SP), Brazil.
Marta Maria da Silva Lira-Batista
Hospital Universitário, Universidade Federal do Piauí - Teresina (PI), Brazil.
Max Morais Pattacini
Hospital da Bahia, DASA - Salvador (BA), Brazil.
Murillo Santucci Cesar de Assunção
Hospital Israelita Albert Einstein - São Paulo (SP), Brazil.
Neymar Elias de Oliveira
Fundação Faculdade Regional de Medicina de São José do Rio Preto - São José do Rio Preto (SP), Brazil.
Oellen Stuani Franzosi
Hospital de Clínicas de Porto Alegre, Universidade Federal do Rio Grande do Sul - Porto Alegre (RS), Brazil.
Patricia Rieken Macedo Rocco
Laboratório de Investigação Pulmonar, Instituto de Biofísica Carlos Chagas Filho, Universidade Federal do Rio de Janeiro - Rio de Janeiro (RJ), Brazil.
Pedro Caruso
AC Camargo Center - São Paulo (SP), Brazil.
Pedro Leme Silva
Laboratório de Investigação Pulmonar, Instituto de Biofísica Carlos Chagas Filho, Universidade Federal do Rio de Janeiro - Rio de Janeiro (RJ), Brazil.
Pedro Vitale Mendes
Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo - São Paulo (SP), Brazil.
Péricles Almeida Delfino Duarte
Universidade Estadual de Ponta Grossa - Ponta Grossa (PR), Brazil.
Renato Fábio Alberto Della Santa Neto
Hospital das Clínicas, Universidade Federal de Pernambuco - Recife (PE), Brazil.
Ricardo Goulart Rodrigues
Hospital do Servidor Público Estadual “Francisco Morato de Oliveira” - São Paulo (SP), Brazil.
Ricardo Luiz Cordioli
Hospital Israelita Alberta Einstein - São Paulo (SP), Brazil.
Roberta Fittipaldi Palazzo
Instituto do Coração, Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo - São Paulo (SP), Brazil.
Rosane Goldwasser
Hospital Universitário “Clementino Fraga Filho”, Universidade Federal do Rio de Janeiro - Rio de Janeiro (RJ), Brazil.
Sabrina dos Santos Pinheiro
Hospital Nossa Senhora Conceição, Grupo Hospitalar Conceição - Porto Alegre (RS), Brazil.
Sandra Regina Justino
Complexo do Hospital de Clínicas, Universidade Federal do Paraná - Curitiba (PR), Brazil.
Sergio Nogueira Nemer
Complexo Hospitalar de Niterói - Rio de Janeiro (RJ), Brazil.
Vanessa Martins de Oliveira
Hospital de Clínicas de Porto Alegre, Universidade Federal do Rio Grande do Sul - Porto Alegre (RS), Brazil.
Vinicius Zacarias Maldaner da Silva
Universidade de Brasília - Brasília (DF), Brazil.
Wagner Luis Nedel
Grupo Hospitalar Conceição - Porto Alegre (RS), Brazil.
Wanessa Teixeira Bellissimo-Rodrigues
Hospital das Clínicas, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo - Ribeirão Preto (SP), Brazil.
Wilson de Oliveira Filho
Hospital Universitário “Getúlio Vargas”, Universidade Federal do Amazonas - Manaus (AM), Brazil.
REFERENCES 1. Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, Gattinoni L, van Haren F, Larsson A, McAuley DF, Ranieri M, Rubenfeld G, Thompson BT, Wrigge H, Slutsky AS, Pesenti A; LUNG SAFE Investigators; ESICM Trials Group. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315(8):788-800.
2. Peñuelas O, Muriel A, Abraira V, Frutos-Vivar F, Mancebo J, Raymondos K, et al. Inter-country variability over time in the mortality of mechanically ventilated patients. Intensive Care Med. 2020;46(3):444-53.
3. Gorman EA, O’Kane CM, McAuley DF. Acute respiratory distress syndrome in adults: diagnosis, outcomes, long-term sequelae, and management. Lancet. 2022;400(10358):1157-70.
4. Rodriguez-Llamazares S, Arroyo-Hernández LJ, Hernández-Cárdenas CM. Mechanical ventilation education for all: call for action. Chest. 2021;159(1):38-9.
5. Brescia D, Pancoast TC, Kavuru M, Mazer M. A survey of fellowship education in mechanical ventilation. Chest. 2008;134(4):s62004.
6. Tallo FS, de Campos Vieira Abib S, de Andrade Negri AJ, Cesar P Filho, Lopes RD, Lopes AC. Evaluation of self-perception of mechanical ventilation knowledge among Brazilian final-year medical students, residents and emergency physicians. Clinics (Sao Paulo). 2017;72(2):65-70.
7. Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149(3 Pt 1):818-24.
8. Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64(4):380-2.
9. Qadir N, Sahetya S, Munshi L, Summers C, Abrams D, Beitler J, et al. An Update on Management of Adult Patients with Acute Respiratory Distress Syndrome: An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2024;209(1):24-36.
10. Grasselli G, Calfee CS, Camporota L, Poole D, Amato MB, Antonelli M, Arabi YM, Baroncelli F, Beitler JR, Bellani G, Bellingan G, Blackwood B, Bos LDJ, Brochard L, Brodie D, Burns KEA, Combes A, D’Arrigo S, De Backer D, Demoule A, Einav S, Fan E, Ferguson ND, Frat JP, Gattinoni L, Guérin C, Herridge MS, Hodgson C, Hough CL, Jaber S, Juffermans NP, Karagiannidis C, Kesecioglu J, Kwizera A, Laffey JG, Mancebo J, Matthay MA, McAuley DF, Mercat A, Meyer NJ, Moss M, Munshi L, Myatra SN, Ng Gong M, Papazian L, Patel BK, Pellegrini M, Perner A, Pesenti A, Piquilloud L, Qiu H, Ranieri MV, Riviello E, Slutsky AS, Stapleton RD, Summers C, Thompson TB, Valente Barbas CS, Villar J, Ware LB, Weiss B, Zampieri FG, Azoulay E, Cecconi M; European Society of Intensive Care Medicine Taskforce on ARDS. ESICM guidelines on acute respiratory distress syndrome: definition, phenotyping and respiratory support strategies. Intensive Care Med. 2023;49(7):727-59.
11. Fan E, Del Sorbo L, Goligher EC, Hodgson CL, Munshi L, Walkey AJ, Adhikari NKJ, Amato MBP, Branson R, Brower RG, Ferguson ND, Gajic O, Gattinoni L, Hess D, Mancebo J, Meade MO, McAuley DF, Pesenti A, Ranieri VM, Rubenfeld GD, Rubin E, Seckel M, Slutsky AS, Talmor D, Thompson BT, Wunsch H, Uleryk E, Brozek J, Brochard LJ; American Thoracic Society, European Society of Intensive Care Medicine, and Society of Critical Care Medicine. An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice Guideline: Mechanical Ventilation in Adult Patients with Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med. 2017;195(9):1253-63.
12. Barbas CS, Ísola AM, Farias AM, Cavalcanti AB, Gama AM, Duarte AC, et al. Brazilian recommendations of mechanical ventilation 2013. Part 2. Rev Bras Ter Intensiva. 2014;26(3):215-39.
13. Barbas CS, Isola AM, Farias AM, Cavalcanti AB, Gama AM, Duarte AC, et al. Brazilian recommendations of mechanical ventilation 2013. Part I. Rev Bras Ter Intensiva. 2014;26(2):89-121.
14. Schmidt GA, Girard TD, Kress JP, Morris PE, Ouellette DR, Alhazzani W, Burns SM, Epstein SK, Esteban A, Fan E, Ferrer M, Fraser GL, Gong MN, L Hough C, Mehta S, Nanchal R, Patel S, Pawlik AJ, Schweickert WD, Sessler CN, Strøm T, Wilson KC, Truwit JD; ATS/CHEST Ad Hoc Committee on Liberation from Mechanical Ventilation in Adults. Official Executive Summary of an American Thoracic Society/American College of Chest Physicians Clinical Practice Guideline: Liberation from Mechanical Ventilation in Critically Ill Adults. Am J Respir Crit Care Med. 2017;195(1):115-9.
15. Schmidt GA, Girard TD, Kress JP, Morris PE, Ouellette DR, Alhazzani W, et al. Liberation From Mechanical Ventilation in Critically Ill Adults: Executive Summary of an Official American College of Chest Physicians/American Thoracic Society Clinical Practice Guideline. Chest. 2017;151(1):160-5.
16. Rochwerg B, Brochard L, Elliott MW, Hess D, Hill NS, Nava S, Navalesi P Members Of The Steering Committee, Antonelli M, Brozek J, Conti G, Ferrer M, Guntupalli K, Jaber S, Keenan S, Mancebo J, Mehta S, Raoof S Members Of The Task Force. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50(2):1602426.
17. Ranzani OT, Bastos LS, Gelli JG, Marchesi JF, Baião F, Hamacher S, et al. Characterisation of the first 250,000 hospital admissions for COVID-19 in Brazil: a retrospective analysis of nationwide data. Lancet Respir Med. 2021;9(4):407-18.
18. Haines A, Kuruvilla S, Borchert M. Bridging the implementation gap between knowledge and action for health. Bull World Health Organ. 2004;82(10):724-31; discussion 732.
19. Davies BL. Sources and models for moving research evidence into clinical practice. J Obstet Gynecol Neonatal Nurs. 2002;31(5):558-62.
20. Miller M, Kearney N. Guidelines for clinical practice: development, dissemination and implementation. Int J Nurs Stud. 2004;41(7):813-21.
21. Cahill NE, Murch L, Cook D, Heyland DK; Canadian Critical Care Trials Group. Improving the provision of enteral nutrition in the intensive care unit: a description of a multifaceted intervention tailored to overcome local barriers. Nutr Clin Pract. 2014;29(1):110-7.
22. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb SA, Beale RJ, Vincent JL, Moreno R; Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580-637.
23. Lane RD, Funai T, Reeder R, Larsen GY. High Reliability pediatric septic shock quality improvement initiative and decreasing mortality. Pediatrics. 2016;138(4):e20154153.
24. Ploeg J, Davies B, Edwards N, Gifford W, Miller PE. Factors influencing best-practice guideline implementation: lessons learned from administrators, nursing staff, and project leaders. Worldviews Evid Based Nurs. 2007;4(4):210-9.
25. Diaz JV, Riviello ED, Papali A, Adhikari NK, Ferreira JC. Global critical care: moving forward in resource-limited settings. Ann Glob Health. 2019;85(1):3.
26. Azevedo LC, Park M, Salluh JI, Rea-Neto A, Souza-Dantas VC, Varaschin P, Oliveira MC, Tierno PF, dal-Pizzol F, Silva UV, Knibel M, Nassar AP Jr, Alves RA, Ferreira JC, Teixeira C, Rezende V, Martinez A, Luciano PM, Schettino G, Soares M; ERICC (Epidemiology of Respiratory Insufficiency in Critical Care) investigators. Clinical outcomes of patients requiring ventilatory support in Brazilian intensive care units: a multicenter, prospective, cohort study. Crit Care. 2013;17(2):R63.
27. Barreira ER, Munoz GO, Cavalheiro PO, Suzuki AS, Degaspare NV, Shieh HH, Martines JA, Ferreira JC, Lane C, Carvalho WB, Gilio AE, Precioso AR; Brazilian Pediatric Acute Respiratory Distress Syndrome Study Group. Epidemiology and outcomes of acute respiratory distress syndrome in children according to the Berlin definition: a multicenter prospective study. Crit Care Med. 2015;43(5):947-53.
28. Ferreira JC, Ho YL, Besen BA, Malbouisson LM, Taniguchi LU, Mendes PV, Costa EL, Park M, Daltro-Oliveira R, Roepke RM, Silva-Jr JM, Carmona MJ, Carvalho CR; EPICCoV Study Group. Protective ventilation and outcomes of critically ill patients with COVID-19: a cohort study. Ann Intensive Care. 2021;11(1):92.
29. Kurtz P, Bastos LS, Dantas LF, Zampieri FG, Soares M, Hamacher S, et al. Evolving changes in mortality of 13,301 critically ill adult patients with COVID-19 over 8 months. Intensive Care Med. 2021;47(5):538-48.
30. Oliveira JP, Costa AC, Lopes AJ, Ferreira AS, Reis LF. Factors associated with mortality in mechanically ventilated patients with severe acute respiratory syndrome due to COVID-19 evolution. Crit Care Sci. 2023;35(1):19-30.
31. Salluh JI, Kurtz P, Bastos LS, Quintairos A, Zampieri FG, Bozza FA. The resilient intensive care unit. Ann Intensive Care. 2022;12(1):37.
32. Soares M, Bozza FA, Angus DC, Japiassú AM, Viana WN, Costa R, et al. Organizational characteristics, outcomes, and resource use in 78 Brazilian intensive care units: the ORCHESTRA study. Intensive Care Med. 2015;41(12):2149-60.
33. Soares M, Salluh JI, Zampieri FG, Bozza FA, Kurtz PM. A decade of the ORCHESTRA study: organizational characteristics, patient outcomes, performance and efficiency in critical care. Crit Care Sci. 2024;36:e20240118en.
34. Hay RE, Martin DA, Rutas GJ, Jamal SM, Parsons SJ. Measuring evidence-based clinical guideline compliance in the paediatric intensive care unit. BMJ Open Qual. 2024;13(1):e002485.
35. Park M, Mendes PV, Zampieri FG, Azevedo LC, Costa EL, Antoniali F, Ribeiro GC, Caneo LF, da Cruz Neto LM, Carvalho CR, Trindade EM; ERICC rese-arch group; ECMO group Hospital Sírio Libanês and Hospital das Clínicas de São Paulo. The economic effect of extracorporeal membrane oxygena-tion to support adults with severe respiratory failure in Brazil: a hypothetical analysis. Rev Bras Ter Intensiva. 2014;26(3):253-62.