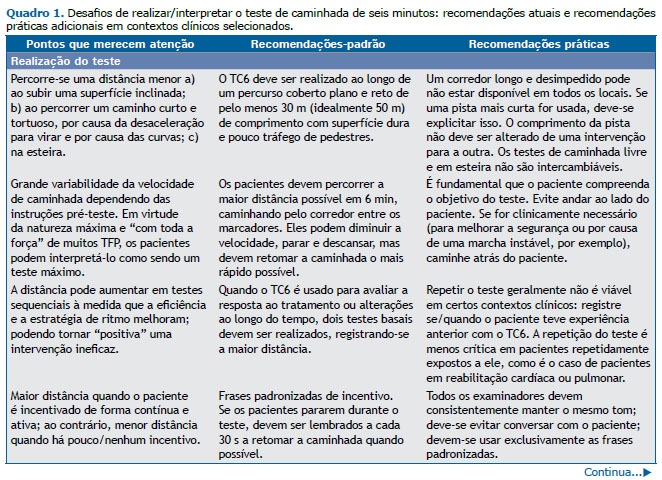
CONTEXTO O teste de caminhada de seis minutos (TC6) foi introduzido na prática clínica há quase meio século. Gradualmente, o TC6 tornou-se o teste clínico de campo mais usado em pacientes com doenças respiratórias crônicas. Não obstante os avanços da padronização,(1,2) existem alguns aspectos referentes à realização e interpretação do teste que devem ser cuidadosamente temperados pelo julgamento clínico individual (Quadro 1).
VISÃO GERAL Uma mulher de 49 anos com IMC = 34,2 kg/m2, síndrome antifosfolípide e dois episódios de embolia pulmonar submaciça evoluiu com hipertensão pulmonar tromboembólica crônica. A distância percorrida no TC6 (DTC6) aumentou de 198 m para 336 m após o início da terapia com riociguate. Nos 6 meses seguintes, a paciente relatou diminuição da tolerância ao exercício: a DLCO, a cintilografia de ventilação/perfusão e o ecocardiograma transtorácico não sugeriram progressão da doença. No entanto, a DTC6 diminuiu em 72 m, isto é, aproximadamente o dobro da diferença mínima clinicamente importante recentemente estimada, de 33 m.(3) Diante dos resultados conflitantes, a paciente foi encaminhada para cateterismo cardíaco direito, que confirmou a estabilidade hemodinâmica. A análise dos resultados do último TC6 revelou o seguinte: a) aumento pronunciado do peso corporal (IMC = 41,2 kg/m2); b) mudança de dispneia para “fadiga dos membros inferiores” do sintoma limitante ao exercício com palpitações, tontura e parestesia nas extremidades; c) SpO2 = 99-100% em ar ambiente. O teste de exercício cardiopulmonar revelou os efeitos negativos da obesidade, descondicionamento físico e disfunção respiratória/hiperventilação. Após emagrecimento agressivo (IMC = 30,7 kg/m2), recondicionamento físico, controle da ansiedade e exercícios respiratórios, a DTC6 aumentou para 389 m, com melhora notável dos sintomas.
O TC6 é um teste de capacidade funcional de caminhar cujo ritmo é determinado pelo próprio paciente e que não fornece nem uma métrica do desempenho/aptidão físicos nem as causas da limitação do exercício. (1,2) Essas considerações não devem impedir o leitor de buscar informações que vão além da DTC6. Por exemplo, no caso aqui relatado, uma análise mais cuidadosa dos achados complementares (progressão da obesidade, sintomas da paciente e SpO2 supranormal em ar ambiente, esta última indicando a presença de descondicionamento e hiperventilação) à luz de outros dados sugerindo estabilidade da doença poderia ter evitado um procedimento invasivo inútil (cateterismo cardíaco direito). O monitoramento contínuo da SpO2 melhora o rendimento da oximetria na previsão de mortalidade e hospitalização em pacientes com DPOC. (4) Paradoxalmente, porém, pode ter consequências indesejáveis, tais como interrupção precoce do exercício e redução da velocidade diante de SpO2 “criticamente baixa” que poderia ser enfrentada na vida diária sem grandes implicações. Os pacientes que experimentam as consequências de longo prazo da dispneia incapacitante e limitação de atividade física têm menos probabilidade de caminhar mais rápido após uma intervenção eficaz: eles “conseguem”, mas não “querem”. De fato, o teste é notoriamente mais sensível a intervenções em pacientes (geralmente mais jovens) com hipertensão arterial pulmonar do que em pacientes mais velhos com DPOC.(2,3)
MENSAGEM CLÍNICA Embora forneça informações limitadas sobre os mecanismos subjacentes à intolerância ao exercício, o TC6 pode ser clinicamente útil para avaliar (a) a capacidade funcional; (b) a gravidade da hipoxemia induzida pela caminhada, incluindo a necessidade de suplementação de O2 durante os esforços; (c) os sintomas que contribuem para a diminuição da tolerância ao exercício; (d) modificações potencialmente significativas da distância percorrida ao longo do tempo, sejam elas espontâneas ou em decorrência de intervenções. De forma semelhante às avaliações mais elaboradas baseadas em exercícios, todos os dados subjetivos e objetivos devem ser interpretados à luz do contexto clínico e das limitações do método (Quadro 1).
REFERÊNCIAS 1. ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test [published correction appears in Am J Respir Crit Care Med. 2016 May 15;193(10):1185]. Am J Respir Crit Care Med. 2002;166(1):111-117. https://doi.org/10.1164/ajrccm.166.1.at1102
2. Holland AE, Spruit MA, Troosters T, Puhan MA, Pepin V, Saey D, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014;44(6):1428-1446. https://doi.org/10.1183/09031936.00150314
3. Moutchia J, McClelland RL, Al-Naamani N, Appleby DH, Blank K, Grinnan D, et al. Minimal Clinically Important Difference in the Six-Minute Walk Distance for Patients with Pulmonary Arterial Hypertension [published online ahead of print, 2023 Jan 11]. Am J Respir Crit Care Med. 2023;10.1164/rccm.202208-1547OC. https://doi.org/10.1164/rccm.202208-1547OC
4. Batista KS, Cézar ID, Benedetto IG, C da Silva RM, Wagner LE, Pereira da Silva D, et al. Continuous Monitoring of Pulse Oximetry During the 6-Minute Walk Test Improves Clinical Outcomes Prediction in COPD. Respir Care. 2023;68(1):92-100. https://doi.org/10.4187/respcare.10091
5. Neder JA. Six-minute walk test in chronic respiratory disease: easy to perform, not always easy to interpret. J Bras Pneumol. 2011;37(1):1-3. https://doi.org/10.1590/S1806-37132011000100001