CONTEXTO A dispneia e a intolerância ao exercício são marcas registradas da hipertensão pulmonar (HP). O conhecimento existente na área advém principalmente de estudos envolvendo pacientes com hipertensão arterial pulmonar. (1) Menos se sabe sobre os determinantes da dispneia aos esforços na HP tromboembólica crônica,(2) causa muito mais frequente de HP na prática clínica.
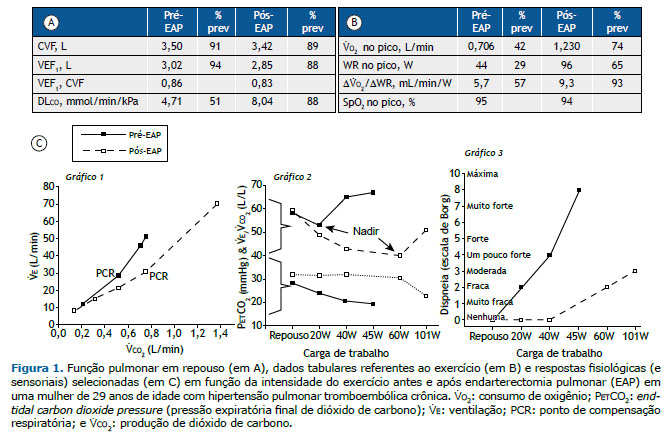
PANORAMA Mulher de 29 anos, não fumante, queixava-se de dispneia progressiva — pontuação na escala modificada do Medical Research Council (mMRC) = 4 — após tromboembolismo pulmonar com alta carga de coágulos dois anos antes. Espirometria normal coexistia com redução moderada da DLCO (Figura 1A). A ecocardiografia revelou HP, e o cateterismo cardíaco direito confirmou HP pré-capilar. Após angiotomografia pulmonar que demonstrou falhas de enchimento residuais nas artérias pulmonares para os lobos inferiores, a paciente foi submetida à endarterectomia pulmonar (EAP). A melhora da dispneia durante as atividades cotidianas (mMRC = 1) após a cirurgia foi acompanhada por um aumento significativo da DLCO (Figura 1A) e do consumo de O2 (V̇O2) em uma determinada taxa de trabalho (WR, do inglês work rate) e no pico do exercício (Figura 1B). A diminuição das demandas de V̇E para uma determinada produção de CO2 (V̇CO2) a partir do início do exercício e a demora para atingir o ponto de compensação respiratória (PCR) para acidose lática foram associadas a menores pontuações de dispneia ao longo do exercício (Figura 1C).
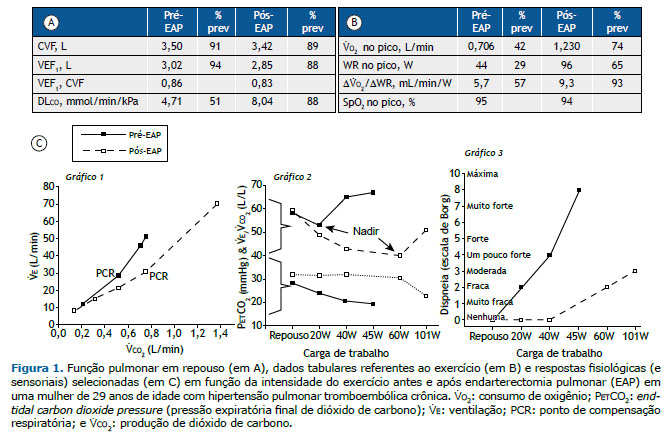
Em indivíduos saudáveis, a eficiência das trocas gasosas pulmonares melhora durante o exercício, uma vez que uma fração menor do VT é desperdiçada no espaço morto (VD, do inglês dead space) fisiológico (anatômico e alveolar; VDfis). Assim, menos V̇E é necessária para eliminar uma determinada quantidade de CO2, isto é, observa-se uma redução no menor valor de V̇E/V̇CO2 (nadir) durante o exercício (Figura 1C, Gráfico 2). Se o VDfis não melhora como esperado (ou até aumenta) (a) e/ou o indivíduo hiperventila diminuindo a PaCO2 (b), a V̇E/V̇CO2 aumenta, trazendo falta de ar.(3) A importância relativa de (a) ou (b) para aumentar a V̇E/V̇CO2 parece variar, dependendo da localização dos coágulos oclusivos: enquanto a doença proximal dos grandes vasos aumenta acentuadamente o VDfis, uma vez que o fluxo sanguíneo é reduzido em boa parte da árvore vascular (a), o aumento na estimulação neuroquímica que leva à hiperventilação (b) tem maior papel contributivo na doença distal dos pequenos vasos.(4) A PCO2 expiratória final é caracteristicamente reduzida na HP tromboembólica crônica (Figura 1C, Gráfico 2, parte inferior) secundária ao comprometimento da perfusão de alvéolos bem ventilados que diminui a taxa de “descarga” de CO2 do sangue venoso misto para os alvéolos (a) e/ou causada por hiperventilação alveolar (b).(5) Na paciente atual, a EAP levou a uma diminuição dramática das demandas ventilatórias durante o exercício (Figura 1C, Gráficos 1 e 2) e melhorou a hemodinâmica central, levando a maior oferta de O2 aos músculos em contração (maior V̇O2/WR), o que retardou o início da acidose metabólica (PCR). Esses fatores, juntamente com pressões vasculares pulmonares mais baixas, provavelmente contribuíram para a diminuição do comando neural respiratório. Em conjunto, esses mecanismos explicam por que a paciente necessitou de 25 L/min a menos de V̇E para eliminar 1 L/min de V̇CO2 a 45 W (a V̇E/V̇CO2 diminuiu de 67 L/L para 42 L/L); consequentemente, a intensidade da dispneia passou de “muito intensa” para “leve” (Figura 1C, Gráfico 3).
MENSAGEM CLÍNICA A diminuição das demandas ventilatórias no exercício tem grandes efeitos benéficos na dispneia em pacientes com HP. As abordagens terapêuticas que melhoram a eficiência das trocas gasosas pulmonares e a função cardiocirculatória (oferta de O2 periférico) permitem a redução do desconforto respiratório, aumentando a tolerância ao exercício dos pacientes.
REFERÊNCIAS 1. Neder JA, Ramos RP, Ota-Arakaki JS, Hirai DM, D’Arsigny CL, O’Donnell D. Exercise intolerance in pulmonary arterial hypertension. The role of cardiopulmonary exercise testing. Ann Am Thorac Soc. 2015;12(4):604-612. https://doi.org/10.1513/AnnalsATS.201412-558CC
2. Ramos RP, Ferreira EVM, Valois FM, Cepeda A, Messina CMS, Oliveira RK, Araújo ATV, et al. Clinical usefulness of end-tidal CO2 profiles during incremental exercise in patients with chronic thromboembolic pulmonary hypertension. Respir Med. 2016;120:70-77. https://doi.org/10.1016/j.rmed.2016.09.020
3. Neder JA, Berton DC, O’Donnell DE. Out-of-proportion dyspnea and exercise intolerance in mild COPD. J Bras Pneumol. 2021;47(3):e20210205. https://doi.org/10.36416/1806-3756/e20210205
4. Zhai Z, Murphy K, Tighe H, Wang C, Wilkins MR, Gibbs JSR, et al. Differences in ventilatory inefficiency between pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension. Chest. 2011;140(5):1284-1291. https://doi.org/10.1378/chest.10-3357
5. Neder JA. Residual Exertional Dyspnea in Cardiopulmonary Disease. Ann Am Thorac Soc. 2020;17(12):1516-1525. https://doi.org/10.1513/AnnalsATS.202004-398FR