ABSTRACT
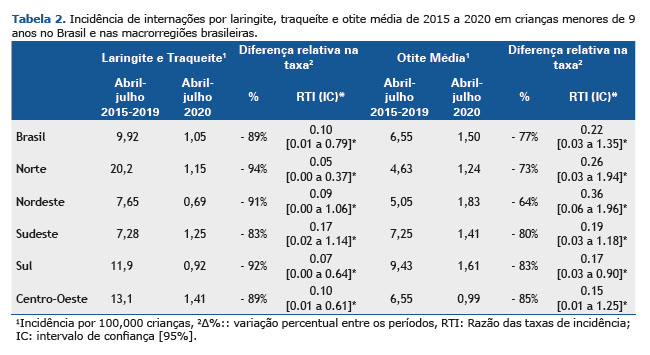
Objective: The objective of this study is to evaluate the impact of social distancing resulting from COVID-19 in hospitalizations for infections of the upper airways (URTI), such as acute laryngitis, tracheitis, and otitis media in children aged 0 to 9 years in Brazil, considering that they share the same forms of transmission. Methods: Data on hospitalizations for acute airway changes and their complications in children <9 years old were obtained from the Database of the Brazilian Department of Public Health Informatics for the period 2015 to 2020. These data were also analyzed by macroregions of Brazil (North, Northeast, Southeast, South, and Midwest). The effect of the social distancing strategy on the increase of acute laryngitis, tracheitis, otitis media, and mastitis, as absolute and relative reductions, was calculated by analyzing the annual calculation of 2015-2019 vs 2020. Results: All the hospitalizations compared in the Unified Health System (SUS) for laryngitis and acute tracheitis and otitis media decreased, considering all states of Brazil. The largest reduction in hospitalization reduction was in the North, with -94% in 2015-2019 vs 2020 in cases of laryngitis and acute tracheitis, and in the Midwest, with - 85% in 2015-2019 vs 2020 in cases of otitis media. Conclusion: Hospitalizations for laryngitis, acute tracheitis, and acute otitis media in children <9 years old decreased between March and July 2020 in Brazil, when social distancing measures were adopted due to the COVID-19 pandemic.
Keywords:
COVID-19; Laryngitis; Otitis media; Confinement; Children; Hospitalization.
RESUMO
Objetivo: O objetivo deste estudo é avaliar o impacto do distanciamento social decorrente da Covid-19 nas internações por infecções das vias aéreas superiores (IVAS), como laringite aguda, traqueíte e otite média em crianças de 0 a 9 anos no Brasil, considerando que compartilham as mesmas formas de transmissão. Métodos: Dados sobre internações por alterações agudas das vias aéreas e suas complicações em crianças <9 anos foram obtidos do Banco de Dados do Departamento Brasileiro de Informática em Saúde Pública para o período de 2015 a 2020. Esses dados também foram analisados por macrorregiões do Brasil (Norte, Nordeste, Sudeste, Sul e Centro-Oeste). O efeito da estratégia de distanciamento social no aumento de laringite aguda, traqueíte, otite média e mastite, como reduções absolutas e relativas, foi calculado analisando o cálculo anual de 2015-2019 vs. 2020. Resultados: Todas as internações comparadas no Sistema Único de Saúde (SUS) por laringite e traqueíte aguda e otite média diminuíram, considerando todos os estados do Brasil. A maior queda na redução de internações foi na região Norte, com -94% em 2015-2019 vs. 2020 nos casos de laringite e traqueíte aguda, e no Centro-Oeste, com -85% em 2015-2019 vs. 2020 nos casos de otite média. Conclusão: As internações por laringite, traqueíte aguda e otite média aguda em crianças <9 anos diminuíram entre março e julho de 2020 no Brasil, quando medidas de distanciamento social foram adotadas devido à pandemia de Covid-19.
Palavras-chave:
COVID-19; Laringite; Otite média; Confinamento; Crianças; Hospitalização.
INTRODUÇÃO Em março de 2020, a Organização Mundial da Saúde (OMS) declarou uma pandemia causada por uma nova espécie de coronavírus, Covid-19 (doença coronavírus 2019). Este surto da doença começou no final de dezembro de 2019, quando pacientes com pneumonia viral devido a um agente microbiano não identificado foram relatados em Wuhan, província de Hubei, China.(1) Por isso, foi publicada a “Atualização da Estratégia Covid-19”, documento produzido pela OMS, no qual são fornecidas orientações aos países de acordo com a mudança epidemiológica esperada com a evolução da pandemia atual. Portanto, as autoridades de saúde tiveram que modificar e implementar algumas medidas para restringir a distância e a circulação ao nível da população, a fim de reduzir a exposição e prevenir a transmissão do vírus.(2)
As infecções das vias aéreas superiores (IVAS) são comumente encontradas em serviços de pronto atendimento pediátrico, principalmente por serem patologias comuns nas infecções respiratórias agudas em crianças. Apresentam transmissibilidade principalmente por meio de gotículas dispersas pela tosse e espirro (como um aerossol) ou mesmo pelo contato de regiões do corpo contaminadas com vias aéreas de indivíduos saudáveis, como as mãos.(3) Por esse motivo, é importante comparar a prevalência dessas doenças em um período de isolamento, uma vez que a disseminação das IVAS ocorre frequentemente em escolas, creches, transportes públicos e outros ambientes públicos, os quais foram fechados ou restritos em relação às recomendações de distância.
Dentre as IRAs mais comuns, destaca-se a laringite viral aguda, também conhecida como crupe viral, que consiste em uma inflamação da parte subglótica da laringe durante a infecção pelo vírus respiratório. O afeto é mais comum em bebês e pré-escolares, com maior incidência aos dois anos de idade. Sua evolução é variável, começando com sintomas de coriza, febre e tosse e progredindo para obstrução leve a grave e dificuldade respiratória. A persistência das vias aéreas geralmente dura de 48 a 72 horas e a regressão ocorre após cinco dias.(3) A maioria dos casos ocorre no outono e no inverno, mas podem se manifestar durante qualquer estação do ano.(4)
A traqueíte bacteriana, por outro lado, é menos comum, mas afeta os tecidos moles da traqueia(5) e também pode se expandir em estruturas subglóticas da laringe e árvore brônquica superior.(6) Os principais agentes infecciosos são bactérias.(7) O afeto é mais comum em crianças durante os primeiros seis anos de vida, tendo os períodos de inverno e outono como os mais proeminentes nos casos, coincidindo com epidemias virais sazonais.(5,8) Os sintomas incluem febre, estridor, tosse, dispneia, odinofagia ou disfagia e alteração da voz.(9)
Outra infecção muito comum na infância é a otite média aguda (OMA), principalmente no período pré-escolar, entre seis meses e três anos de idade,(10) caracterizada por dor de ouvido, otite, febre, agitação noturna, diminuição da ingestão alimentar e sonolência.(11) É um processo inflamatório, que pode ser viral ou bacteriano e geralmente ocorre devido a uma complicação de infecção das vias aéreas superiores (IVAS). Os fatores de risco para tal infecção são exposição à fumaça, uso de mamadeiras e chupetas, posição supina e, principalmente, cuidados na creche.(10)
Portanto, é importante destacar que o período de início das medidas restritivas devido à pandemia de Covid-19 no Brasil ocorreu em fevereiro de 2020, pouco antes do outono do hemisfério sul, e permaneceu durante todo o inverno (de março a setembro), período em que há maior incidência das patologias descritas acima. Na China, no mesmo período, estudos mostraram uma diminuição concomitante de influenza, enterovírus e pneumonia. Portanto, a implementação de medidas de controle de infecção, incluindo o uso de máscaras, higienização das mãos e distanciamento social para prevenir a disseminação da Covid-19, pode ter tido um forte impacto na redução da disseminação de outros patógenos infecciosos em pediatria.(12-15) Portanto, o objetivo deste estudo é avaliar o impacto precoce do distanciamento social devido à Covid-19 e hospitalizações por laringite aguda, traqueíte e otite média em crianças de 0 a 9 anos no Brasil.
MÉTODOS O delineamento utilizado foi um estudo ecológico, no qual foram obtidos dados de internações por laringite e otite do banco de dados do Departamento de Informática do Sistema Único de Saúde (DATASUS) (16) que fornece o diagnóstico de internação para o período 2015-2020 (mês a mês). O DATASUS apresenta números absolutos de internações na rede pública, obtidos de acordo com a Classificação Internacional de Doenças, versão 10 (CID-10). Considera o principal diagnóstico em hospitalização, podendo armazenar informações com cobertura universal da população brasileira.(17) Para acessar os dados, os links “Informações em Saúde” (TABNET) - “Epidemiológica e Morbidade” (Epidemiologia e Morbidade) - “Morbidade Hospitalar” (Morbidade Hospitalar), “Lista de Morbidade” (Lista de Morbidade), respectivamente para o faixa etária de 0 a 9 anos. Esses dados também foram analisados pelas macrorregiões do Brasil (Norte, Nordeste, Sudeste, Sul e Centro-Oeste), devido às variações na densidade populacional, variação climática e fatores socioeconômicos, considerando a extensão continental do país. Foram pesquisados os meses de janeiro a junho de cada ano, pois abrangem os períodos de alta típica em internações por laringite, traqueíte aguda, otite média e outros distúrbios do processo médio e mastóide. Para avaliar a confiabilidade do relato, neoplasia maligna do osso e da cartilagem articular foi usada como comparação, uma vez que não se espera que as medidas de distância social tenham um grande impacto nessas condições.
Por se tratar de uma busca de dados em plataforma disponível online, com dados alimentados pelo Sistema Único de Saúde, sem identificação pessoal do paciente, não foi necessária a análise e aprovação do Comitê de Ética em Pesquisa. A ferramenta, portanto, conta com o número de internações que podem ser estratificadas de acordo com a idade e localidade.
Para avaliar o efeito das medidas de contenção da pandemia sobre a incidência das doenças acima mencionadas, a redução absoluta (sem e com medidas de contenção da pandemia) e a redução relativa (sem e com medidas de contenção da pandemia) foram calculadas através da análise dos subconjuntos 2015-2019 vs. 2020. Assim, foram feitas duas análises: a primeira visando uma análise geral do panorama, observando os meses de janeiro a julho, e outra para avaliar o efeito do distanciamento social, com abril a julho. Março foi o mês de corte por ser o período de implementação das medidas de contenção da pandemia no Brasil em 2020 e a partir de abril o período de maior impacto.(18) Para garantir a qualidade da coleta, dois autores independentes revisaram os dados.
O cálculo da incidência mensal de internações no sistema público de saúde utilizou a fórmula: número total de internações / número populacional por idade (por ano e local [Brasil-IBGE]) x 100.000 habitantes.(19) O seguro saúde a cada ano, fornecido pela Agência Nacional de Saúde, variou de 20,80% em 2015 a 19,60% em 2020 para a população com menos de 14 anos durante o período do estudo.(20) Esse percentual foi excluído do denominador, pois a população pode fazer uso de outros meios hospitalares e os dados de internação não estão incluídos no DATASUS. Para calcular a diferença de incidência entre os períodos pandêmicos com e sem medidas de contenção, foi utilizada a razão das taxas de incidência (RTI) para avaliar a significância estatística, com intervalo de confiança de 95%.
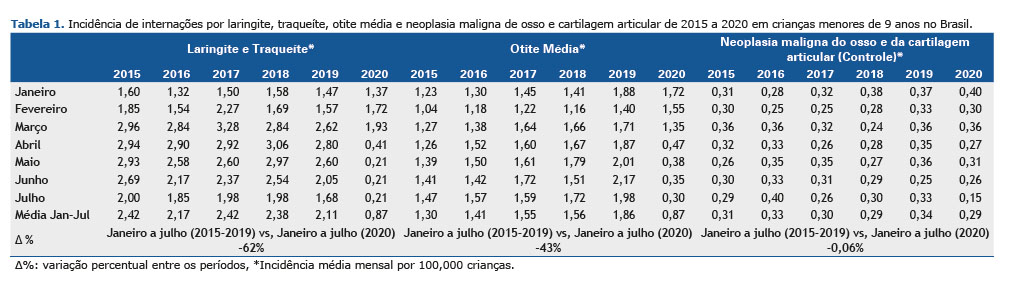
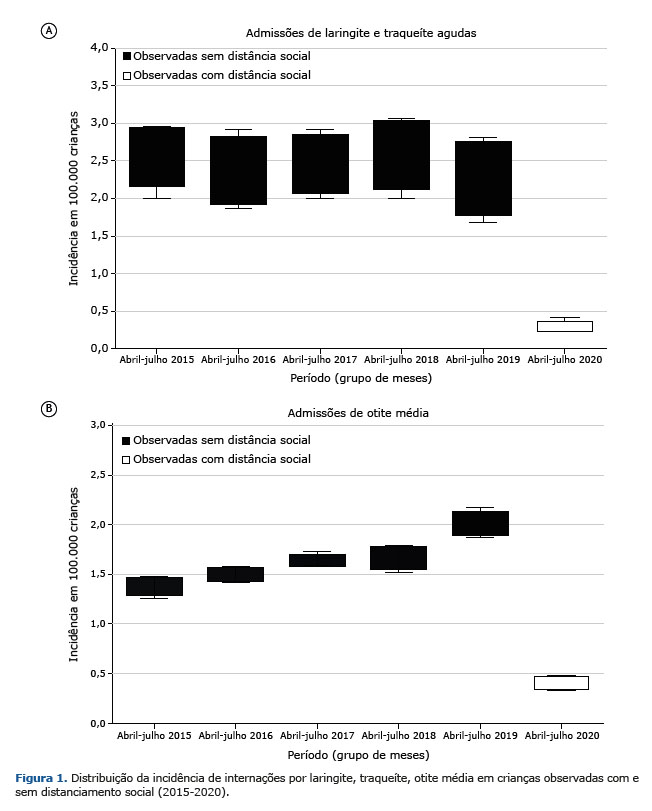
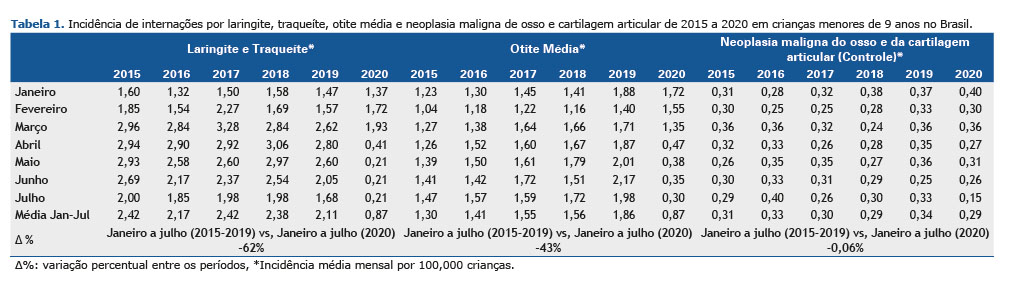
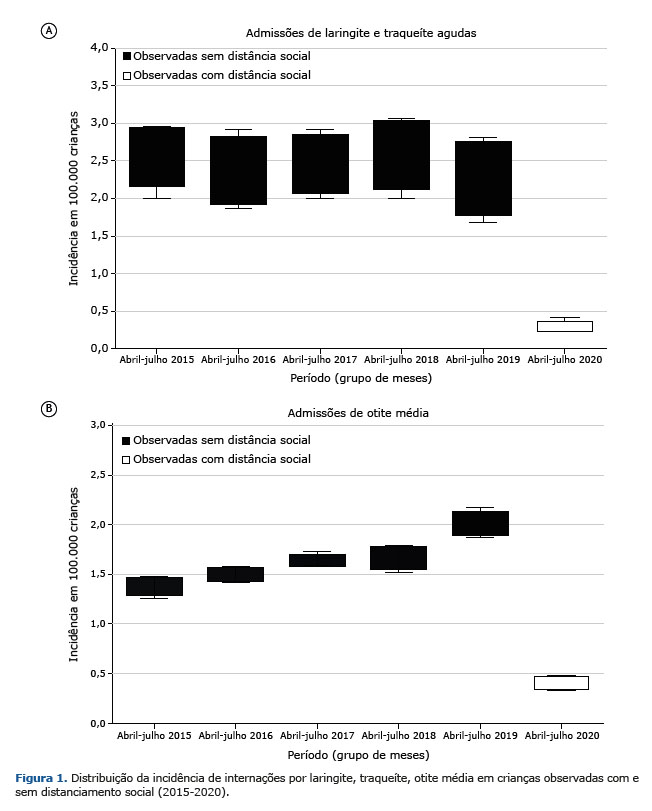
RESULTADOS Com base nas internações no Sistema Único de Saúde (SUS), por meio de informações do banco de dados, a distribuição mensal da incidência de internações por laringite e traqueíte aguda no período de janeiro a fevereiro foi semelhante, com tendência de redução ao longo do período de estudo. (2015-2020). A menor incidência foi observada em janeiro de 2016, com 1,32 / 100.000 internações, e a maior em fevereiro de 2017, com 2,27 / 100.000 internações. No período entre março e abril, a tendência de queda foi mantida, mas com picos de internações, principalmente em março de 2017, com 3,28 / 100.000 internações, e abril de 2018, com 3,06 / 100.000 internações, sendo a menor incidência registrada neste período de abril de 2020, com 0,41 / 100.000 internações. O mês de maio, durante os anos analisados, manteve um padrão linear e queda acentuada em 2020. A maior incidência foi de 2,97 / 100.000 em 2018 e a menor foi de 0,21 / 100.000 em 2020. Junho manteve uma incidência muito próxima em 2015, 2016, 2017 e 2018, com queda na incidência em 2019; entretanto, em 2020, esse mês apresentou queda significativa nesse parâmetro, queda que vinha ocorrendo desde abril, com 0,41 / 100.000 internações para 0,21 / 100.000 em maio, junho e julho. No período entre janeiro e julho de 2015 a 2020, a incidência de laringite e traqueíte aguda foi de 2,42 / 100.000 (2015), 2,17 / 100.000 (2016), 2,42 / 2100.000 (2017), 2,38 / 100.000 (2018), 2,11 / 100.000 (2019), 0,87 / 100.000 (2020), respectivamente.
Em relação à distribuição mensal da incidência de internações por otite média, os meses de janeiro a março apresentaram valores semelhantes, com tendência de aumento ao longo do período estudado (2015-2020). A menor incidência foi observada em fevereiro de 2015, com 1,04 / 100.000 internações, e a maior em janeiro de 2019, com 1,88 / 100.000 internações. Os meses de abril e maio, nos anos analisados, mantiveram aumento linear, mas queda acentuada em 2020. A maior incidência foi de 2,01 / 100.000 em 2019 e a menor foi de 0,38 / 100.000 em 2020. O mesmo padrão é observado mantido em julho, com aumento das incidências de 2015 a 2019, com maior incidência registrada em 2019, com 1,98 / 100.000, mas com queda acentuada em 2020, chegando a 0,30 / 100.000. No período entre janeiro e julho de 2015 a 2020, a incidência de otite média foi de 1,30 / 100.000 (2015), 1,41 / 100.000 (2016), 1,55 / 10.000 (2017), 1,56 / 100.000 (2018), 1,86 / 100.000 (2019), 0,87 / 100.000 (2020), respectivamente, conforme mostrado na Tabela 1.
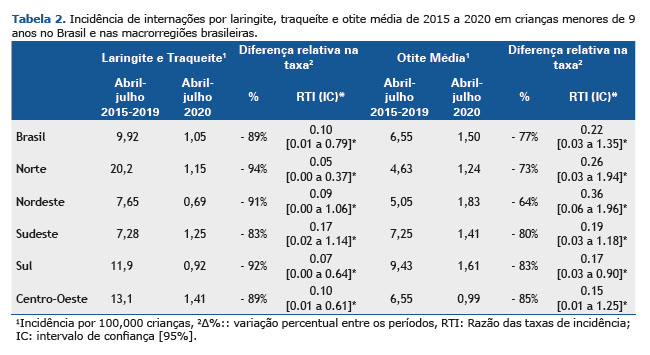
Na comparação dos subconjuntos por macrorregiões do Brasil sobre laringite e traqueíte aguda (abril a julho de 2015 a abril a julho de 2020), também houve redução significativa em todas as comparações. A região Norte apresentou a maior redução na incidência de internações, com -94% [RTI 0,05 (0,00 a 0,37)] no período 2015-2019 vs. 2020. No Nordeste, a redução variou -91% [RTI 0,09 (0,00 a 1,06)] no período 2015-2019 vs. 2020. Para a região Sudeste, houve redução de -83% [RTI 0,17 (0,02 para 1,14)] no período 2015-2019 vs. 2020. A região Sul mostrou uma redução na incidência, variando -92% [RTI 0,07 (0,00 a 0,64)] em 2015-2019 vs. 2020. Na região Centro-Oeste, a variação foi de -89% [RTI 0,10 (0,01 a 0,61)] no período 2015-2019 vs. 2020 na incidência de internações.
Nos subconjuntos por macrorregiões do Brasil, na comparação com otite média (abril a julho de 2015 a 2019 vs. abril a julho de 2020), houve queda significativa e relevante em todas as comparações. Na região Norte, a redução na incidência de internações foi de -73% [RTI 0,26 (0,03 para 1,94)] no período 2015-2019 vs. 2020. No Nordeste, a redução variou de -64% [RTI 0,36 (0,06 a 1,96)] no período 2015-2019 vs. 2020. Para a região Sudeste, houve redução de -80% [RTI 0,19 (0,03 para 1,18)] no período 2015-2019 vs. 2020. A região Sul apresentou redução na incidência de -83% [RTI 0,17 (0,03 a 0,90)] em 2015-2019 vs. 2020. A região Centro-Oeste apresentou a maior variação, com -85% [RTI 0,15 (0,01 a 1,25)] no período 2015-2019 vs. 2020 na incidência de internações. O número total absoluto de internações, a incidência de internações por 100.000 habitantes (0 a 9 anos) e as diferenças entre as internações no período entre 2015 e 2020 são apresentados na Tabela 2. A Figura 1 resume os resultados encontrados neste estudo.
Por meio dos dados obtidos pelo DATASUS e de sua análise ao longo dos anos no Brasil, este estudo tem como objetivo avaliar os impactos de medidas aplicadas ao distanciamento social, a fim de reduzir a incidência de internações pediátricas em crianças de 0 a 9 anos por infecções das vias aéreas superiores. Tais intervenções, implementadas pelo Ministério da Educação do Brasil, para controlar a disseminação viral em ambientes como escolas e creches entraram em vigor no dia 17 de março, próximo ao início do outono no hemisfério sul, quando costuma haver um significativo aumento das internações por laringite, traqueíte aguda e otite média na população pediátrica.(4) Além disso, devido ao elevado índice populacional e ao fato de que o período de implementação das medidas a distância coincide com o período em que os agentes causadores das doenças acima mencionadas, os dados epidemiológicos apresentam inúmeras vantagens em termos de qualidade.(21)
Considerando dados do Centro de Controle e Prevenção de Doenças (CDC), uma agência do Departamento de Saúde e Serviços Humanos dos EUA, as hospitalizações por Covid-19 na população pediátrica são extremamente incomuns — cerca de 4,1%. Esses dados diminuem ainda mais quando se trata da necessidade de uma unidade de terapia intensiva (UTI) pediátrica para indivíduos da mesma faixa etária — menos de 1%. Tais taxas também foram observadas em outros países desenvolvidos, como China, Itália, França e Espanha, que mantêm um padrão muito semelhante. Na França, por exemplo, François Angoulvant, médico pediatra de emergência, coletou informações sobre visitas a seis prontos-socorros de crianças em Paris a partir de março de 2020, quando o governo francês ordenou o fechamento parcial da região por conta da chegada da Covid-19. Foram analisados dados de 871.500 pacientes entre 2017 e 2020, nos quais as internações em prontos-socorros pediátricos diminuíram 45% durante os meses da pandemia.(22) O Brasil, por sua vez, apresentou, por meio de estudo recente, 56% das internações hospitalares na população pediátrica, dentre as quais 19% necessitaram de UTIP nos casos de Covid-19; entretanto, este estudo analisou hospitais de referência de alta complexidade clínica e, portanto, pacientes com múltiplas comorbidades, o que pode ser o motivo de tal desvio acentuado quando comparado a estudos em países desenvolvidos. Embora uma revisão sistemática de Hoang et al. em 2020 tenha identificado coinfecção em 6% dos casos de internação pediátrica com Mycoplasma pneumonia e Vírus Sincicial Respiratório, muitos estudos apontam para uma diminuição significativa em várias regiões do mundo no tratamento das doenças mencionadas e suas respectivas internações em pediatria.(23) O estudo Yeoh et al.(24)) analisou a população pediátrica da Austrália e mostrou reduções de 98,0% e 99,4% nas detecções de VSR e influenza, respectivamente, até o inverno de 2020, assim como um estudo realizado na Bélgica mostrou uma diminuição de >99% nos casos registrados de VSR em 2020 em comparação com os anos anteriores.(25) Este fato pode estar intimamente ligado, porque a transmissibilidade dos agentes respiratórios diminuiu devido às medidas de isolamento, com uma consciência geral da necessidade de lavagem adequada das mãos, uso de álcool gel, limpeza regular de brinquedos, uso individual de utensílios e máscaras pessoais, além do fechamento de escolas e clubes esportivos propostos pelo governo brasileiro.(26,27) Portanto, todas as medidas mencionadas podem ter contribuído para a redução da laringite, traqueíte e otite média aguda em crianças, reduzindo o contato interpessoal e maiores cuidados com a higiene pessoal.
De acordo com a Sociedade Brasileira de Pediatria, é necessário haver cuidadosa manutenção dos cuidados às crianças e adolescentes, mesmo em tempos de pandemias. Segundo dados da FIOCRUZ — principal instituição não universitária de formação e qualificação de recursos humanos para o SUS e à área de ciência e tecnologia no Brasil(28) —, algumas unidades de saúde registraram redução no número de atendimentos ambulatoriais de até 90% entre março e julho de 2020, quando comparado ao mesmo período de 2019, causando diversos prejuízos ao paciente e futura superlotação nos serviços de saúde do país.(22) Esse fato também foi analisado por meio de um estudo multicêntrico recente, que mostrou que as visitas de emergência e as internações hospitalares foram bastante reduzidas durante os bloqueios de Covid-19 na Holanda, como no resto do mundo, especialmente para crianças com infecções transmissíveis.(29) Embora seja amplamente conhecido que esse período de isolamento tem trazido problemas de saúde quando se trata de visitas de rotina ou acompanhamento de doenças crônicas, é possível observar que as medidas propostas pelas diretrizes para o controle da transmissão da SARS-CoV -2 impactou outros agentes etiológicos, que estão relacionados à laringite, traqueíte e otite média.(27,30,31) Esse achado corrobora a hipótese de que as medidas de saúde não farmacológicas para conter a pandemia de Covid-19 têm um impacto significativo na disseminação de vários vírus respiratórios.
Houve queda acentuada nas taxas de internações entre março e julho de 2020 em todas as macrorregiões brasileiras, período em que foram implementadas medidas restritivas.(2) Nossos achados mostram que, anualmente, a incidência de hospitalizações por laringite, traqueíte aguda e otite média aumenta, como ocorre em países em desenvolvimento, como o Brasil. No entanto, nota-se que houve uma redução drástica na incidência de internações pediátricas por infecções das vias aéreas superiores no período de 2015-19 a 2020 a partir de março, quando no Brasil teve início o distanciamento social devido à Covid-19. Antes desse período, ou seja, em janeiro e fevereiro de 2020, havia incidência semelhante ao longo dos anos, com aumento exponencial dos casos de internação, considerando a sazonalidade da doença no país.(32) Para hospitalizações por laringite e traqueíte aguda, os dados sugerem uma tendência de queda ao longo do período de estudo (2015-2020). A menor incidência ocorreu em abril de 2020 e essa redução significativa foi mantida em maio e junho. Nas internações por otite média aguda, houve tendência de alta no período de 2015 a 2020. Os meses de janeiro a março mantiveram valores semelhantes, mas de abril a julho, o aumento observado até 2019 foi interrompido por uma queda acentuada no ano 2020. Na comparação entre as macrorregiões brasileiras, a região Norte apresentou maior redução nas internações por laringite e traqueíte aguda (-94%). Em segundo lugar, a região Sul recuou -92%, seguida pelo Nordeste (-91%), Centro-Oeste (-89%) e Sudeste (-83%). Quanto às internações por otite média aguda, houve queda acentuada em todas as comparações, a mais significativa na região Centro-Oeste (-85%). A região Sul caiu -83% e foi seguida por Sudeste (-80%), Norte (-73%) e Nordeste (-64%).
Por fim, o presente estudo retrospectivo, entretanto, apresenta algumas limitações, como a impossibilidade de avaliação de intervenções não farmacológicas isoladas, por serem realizadas simultaneamente. Em termos de coleta de dados, outra limitação diz respeito à plataforma, pois foram preenchidos por terceiros, funcionários do DATASUS, e não pelos pesquisadores que os redigiram, considerando o período pandêmico e a distância social. Os dados foram coletados a cada mês com um atraso de dois meses e, de acordo com nossas experiências anteriores, este período é suficiente para o DATASUS atualizar os números finais ou os valores muito aproximados, considerando que os dados estão incluídos de acordo com os formulários de Autorizações de Internação, no Brasil AIH (Autorização de Internação Hospitalar). Ainda a esse respeito, os dados apresentam caráter populacional, com informações epidemiológicas nacionais e regionais robustas, levando-se em consideração o porte populacional, o que reitera os achados e se apresenta como uma vantagem em relação aos demais estudos. (33,34) Além disso, ao analisarmos as internações por otites, estamos cobrindo apenas os casos graves, visto que os casos mais leves e mais comuns recebem tratamento ambulatorial, o que pode representar um viés em termos de estimativa da queda real da incidência dessa infecção. No entanto, e com tais limitações, consideramos que esses resultados refletem verdadeiramente o momento atual, visto que foram os mesmos durante todo o período de avaliação, o que reforça a validade dos principais achados do presente estudo. Tais mudanças no perfil das internações pediátricas, do ponto de vista epidemiológico, não haviam sido relatadas antes no Brasil.
AGRADECIMENTOS Os autores agradecem às instituições de saúde do Brasil que desenvolveram o banco de dados DATASUS e o disponibilizaram para pesquisa: Departamento de Informática do Sistema Único de Saúde e Ministério da Saúde.
CONTRIBUIÇÃO DOS AUTORES CRJ participou do planejamento do estudo, coordenou a coleta de dados e redigiu o artigo. AASR, ASM, ACA, FBM, SMF, LCSM participaram do planejamento, coleta de dados e redação da primeira versão do paper. Frederico Friedrich participou da análise e redação final do artigo. LAP coordenou o planejamento do estudo, a coleta de dados e redação final do artigo.
REFERÊNCIAS 1. WHO: World Health Organization [Internet]. WHO Director-General’s opening remarks at the media briefing on COVID-19. Switzerland: WHO; 2020 [cited 2020 Nov 5]. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
2. WHO: World Health Organization [Internet]. COVID19 strategy update. Switzerland: WHO; 2020 [cited 2020 Nov 5]. Available from: https://www.who.int/publications/i/item/covid-19-strategy-update---14-april-2020
3. Pitrez Paulo MC, Pitrez José LB. Acute upper airway infections: diagnosis and outpatient treatment. J Pediatr J River. [serial on the Internet]. 2003 June [cited 2020 Oct 21];79(Suppl 1):S77-86. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0021-75572003000700009&lng=en
4. SBP: Sociedade Brasileira de Pediatria [Internet]. Crupe viral e bacteriano. Guia Prático de Conduta. Departamento de Emergências; 2017 [cited 2020 Oct 24]. p. 1-9. Available from: https://www.sbp.com.br/fileadmin/user_upload/2017/01/Emergncia-Crupe-Viral-e-Bacteriano.pdf
5. Jones R, Santos JI, Overall JC Jr. Bacterial tracheitis. JAMA. 1979;242(8):721-6. http://dx.doi.org/10.1001/jama.1979.03300080019018. PMid:379379.
6. Conley SF, Beste DJ, Hoffmann RG. Measles-associated bacterial tracheitis. Pediatr Infect Dis J. 1993;12(5):414-5. http://dx.doi.org/10.1097/00006454-199305000-00017. PMid:8327305.
7. Hjuler IM, Hansen MB, Olsen B, Renneberg J. Bacterial colonization of the larynx and trachea in healthy children. Acta Paediatr. 1995;84(5):566-8. http://dx.doi.org/10.1111/j.1651-2227.1995.tb13696.x. PMid:7633155.
8. Wood CR. Bacterial tracheitis in children: clinical characteristics and diagnosis [Internet]. UpToDate; 2019 [cited 2020 Oct 6]. Available from: https://www.uptodate.com/contents/bacterial-tracheitis-in-children-clinical-features-and-diagnosis?search=traqueite%20acute&source=search_result&selectedTitle=1~18&usage_type=default&display_rank=1#H23
9. Casazza G, Graham ME, Nelson D, Chaulk D, Sandweiss D, Meier J. Pediatric bacterial tracheitis-a variable entity: case series with literature review. Otolaryngol Head Neck Surg. 2019;160(3):546-9. http://dx.doi.org/10.1177/0194599818808774. PMid:30348058.
10. Di Francesco RC, Moricz RD, Marone S. Otite média aguda em pediatria: diagnóstico e tratamento. Boletim da Sociedade de Pediatria de São Paulo [serial on the Internet]. 2016 [cited 2020 Oct 28];1(3):4-6. Available from: https://www.spsp.org.br/site/asp/boletins/AT3.pdf
11. Venekamp RP, Damoiseaux RA, Schilder AG. Acute otitis media in children. BMJ Clin Evid. 2014. [cited 2014 Sep 16];09:301. PMID: 25229555. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4166866/pdf/2014-0301.pdf.
12. Friedrich F, Ongaratto R, Scotta MC, Veras TN, Stein RT, Lumertz MS, et al. Early Impact of social distancing in response to Coronavirus Disease 2019 on hospitalizations for acute bronchiolitis in infants in Brazil. Clin Infect Dis. 2021;72(12):2071-5. http://dx.doi.org/10.1093/cid/ciaa1458. PMid:32986818.
13. Edwards KM. The impact of social distancing for SARS-CoV-2 on respiratory syncytial virus and Influenza Burden. Clin Infect Dis. 2020;72(12):2076-8. http://dx.doi.org/10.1093/cid/ciaa1543.
14. Fong MW, Gao H, Wong JY, Xiao J, Shiu EYC, Ryu S, et al. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings-social distancing measures. Emerg Infect Dis. 2020;26(5):976-84. http://dx.doi.org/10.3201/eid2605.190995. PMid:32027585.
15. Varela FH, Scotta MC, Polese-Bonatto M, Sartor ITS, Ferreira CF, Fernandes IR, et al. Absence of detection of RSV and influenza during the COVID-19 pandemic in a Brazilian cohort: likely role of lower transmission in the community. J Glob Health. 2021;11:05007. http://dx.doi.org/10.7189/JOGH.11.05007. PMid:33791096.
16. Brazil. DATASUS: Ministry of Health. Health Information (TABNET). [cited 2020 Jun 23]. Available at: https://datasus.saude.gov.br/informacoes-de-saude-tabnet/.
17. Sousa AF, Stadulni ARP, Costa LBA. Uso de dados do departamento de informática do Sistema Único de Saúde (DATASUS) em pesquisas científicas. Rev Multidiscip Núcleo do Conhecimento. 2021;11:171-85. http://dx.doi.org/10.32749/nucleodoconhecimento.com.br/saude/saude-datasus
18. Brasil. Lei nº 13.979, de 6 de Fevereiro de 2020. Dispõe sobre as medidas para enfrentamento da emergência de saúde pública de importância internacional decorrente do coronavírus responsável pelo surto de 2019. Diário Oficial da União; Brasília; 2020.
19. IBGE: Instituto Brasileiro de Geografia e Estatística [Internet]. Projeções da população. Rio de Janeiro: IBGE; 2018 [cited 2020 June 8]. Available from: https://www.ibge.gov.br/estatisticas/sociais/populacao/9109-projecao-da-populacao.html?edicao=21830&t=resultados
20. Brazil. ANS: National Supplementary Health Agency. TABNET [Internet]. [cited 2020 Jun 23]. Available from: https://www.gov.br/ans/pt-br.
21. Brasil. Ministério da Educação. Portaria nº 343, de 17 de Março de 2020. Dispõe sobre a substituição das aulas presenciais por aulas em meios digitais enquanto durar a situação de pandemia do Novo Coronavírus - COVID-19 [Internet]. Diário Oficial da União; Brasília; 2020 [cited 2021 Jan 18]. Available from: https://www.in.gov.br/en/web/dou/-/portaria-n-343-de-17-de-marco-de-2020-248564376
22. Angoulvant F, Ouldali N, Yang DD, Filser M, Gajdos V, Rybak A, et al. COVID-19 pandemic: Impact caused by school closure and national blockade on pediatric visits and hospitalizations for viral and non-viral infections, a time series analysis. Clin Infect Dis. 2020 Jun 3:ciaa710. PMID: 33501967.
23. Instituto Fernandes Figureira. COVID-19 e saúde da criança e do adolescente [Internet]. Rio de Janeiro: IFF; 2020 [cited 2021 Jan 20]. p. 1-70. Available from: http://www.iff.fiocruz.br/pdf/covid19_saude_crianca_adolescente.pdf
24. Yeoh DK, Foley DA, Minney-Smith CA, Martin AC, Mace AO, Sikazwe CT, et al. The impact of COVID-19 public health measures on detections of influenza and respiratory syncytial virus in children during the 2020 Australian winter. Clin Infect Dis. 2021;72(12):2199-202. http://dx.doi.org/10.1093/cid/ciaa1475. PMid:32986804.
25. Van Brusselen B, De Troeyer K, ter Haar E, Auwera AV, Poschet K, Van Nuijs S, et al. Bronchiolitis in COVID-19 times: a nearly absent disease? Eur J Pediatr. 2021;180:1969-73. http://dx.doi.org/10.1007/s00431-021-03968-6.
26. Brasil. Ministério da Saúde. Saúde anuncia orientações para evitar a disseminação do coronavírus [Internet]. Brasília: Ministério da Saúde; 2020 [cited 2021 Jan 31]. Available from: https://www.gov.br/saude/pt-br/assuntos/noticias/saude-anuncia-orientacoes-para-evitar-a-disseminacao-do-coronavirus
27. Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM, et al. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014;134(5):e1474-502. http://dx.doi.org/10.1542/peds.2014-2742. PMid:25349312.
28. Fiocruz: Fundação Oswaldo Cruz. Pesquisa e ensino [Internet]. 2021 [cited 2021 Jan 18]. Available from: https://portal.fiocruz.br/pesquisa-e-ensino#:~:text=A%20Fiocruz%20%C3%20%20main,e%20v%C3%A1rios%20programs%20lato%20sensu
29. Kruizinga MD, Peeters D, van Veen M, van Houten M, Wieringa J, Noordzij JG, et al. The impact of lockdown on pediatric ED visits and hospital admissions during the COVID19 pandemic: a multicenter analysis and review of the literature. Eur J Pediatr. 2021;180(7):2271-9. http://dx.doi.org/10.1007/s00431-021-04015-0. PMid:33723971.
30. Angoulvant F, Ouldali N, Yang DD, Filser M, Gajdos V, Rybak A, et al. Coronavirus Disease 2019 Pandemic: Impact caused by school closure and national lockdown on pediatric visits and admissions for viral and nonviral infections - a time series analysis. Clin Infect Dis. 2021;72(2):319-22. http://dx.doi.org/10.1093/cid/ciaa710. PMid:33501967.
31. Erlichman M, Zalut T, Schwartz S, Weiser G. The ongoing indirect effect of the COVID 19 pandemic on a pediatric emergency department. PLoS One. 2021;16(5):e0251003. http://dx.doi.org/10.1371/journal.pone.0251003.
32. Pedreira BAM. Fatores de risco para hospitalização por infecção respiratória aguda em crianças [Internet]. Salvador: Universidade Federal da Bahia; 2013 [cited 2021 Jan 18]. Available from: https://repositorio.ufba.br/ri/bitstream/ri/12830/1/DISS.%20BETANIA%202013.pdf
33. Friedrich F, Valadão MC, Brum M, Comaru T, Pitrez PM, Jones MH, et al. Impact of maternal dTpa vaccination on the incidence of pertussis in young infants. PLoS One. 2020;15(1):e0228022. http://dx.doi.org/10.1371/journal.pone.0228022.
34. Scotta MC, Veras TN, Klein PC, Tronco V, Polack FP, Mattiello R, et al. Impact of 10-valent pneumococcal non-typeable Haemophilus influenzae protein D conjugate vaccine (PHiD-CV) on childhood pneumonia hospitalizations in Brazil two years after introduction. Vaccine. 2014;32(35):4495-9. http://dx.doi.org/10.1016/j.vaccine.2014.06.042. PMid:24958703.