AO EDITOR,A DPOC é caracterizada por sintomas respiratórios persistentes, como dispneia, que contribui para a limitação ao exercício. Dentre os fatores envolvidos nesses mecanismos, destaca-se a disfunção muscular respiratória.(1) Portanto, alterações nos volumes e capacidades pulmonares, principalmente a redução da CV e a fraqueza dos músculos respiratórios, podem ser observadas nessa população de pacientes.(2)
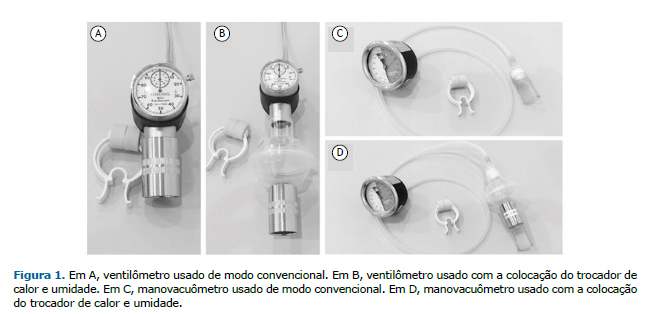
A mensuração da CV e das pressões respiratórias (PImáx e PEmáx) é realizada por meio de um ventilômetro (Figura 1A) e um manovacuômetro (Figura 1C), respectivamente. Esses equipamentos são higienizados apenas externamente, podendo contribuir para o aumento da incidência de infecções, visto que, durante as avaliações de rotina, nenhum dispositivo é empregado para filtrar o ar inspirado e expirado pelo paciente.(3) Portanto, uma alternativa viável seria utilizar o heat and moisture exchangers (HMEs, trocadores de calor e umidade) nesses equipamentos.
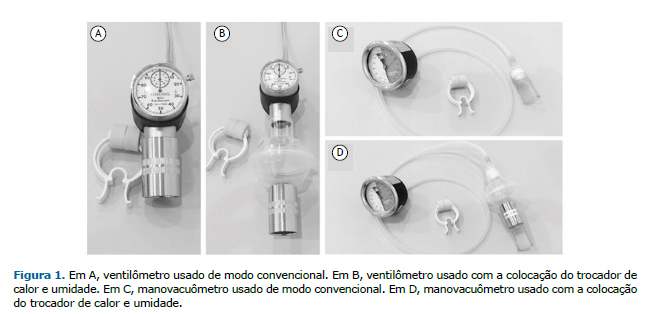
O HME hidrofóbico tem um filtro microbiológico que reduz a contaminação dos aparelhos (Figuras 1B e 1D), protegendo os pacientes da contaminação microbiana.(4)
Lucato et al.(5) demonstraram que o volume do espaço morto e a resistência causados pela adição do HME não modificou os valores de CV e da força muscular respiratória em voluntários avaliados em respiração espontânea. Estudos focando pacientes com alterações da função pulmonar para verificar se a adição do filtro leva a um impacto relevante nesses resultados não foram feitos anteriormente, mas são importantes, já que alguns estudos relatam que o HME pode levar a um aumento da resistência,(6) e essa resistência pode causar problemas em pacientes com DPOC.
O objetivo do presente estudo foi avaliar se o uso do HME com filtro microbiológico interfere nas medidas de pressões respiratórias máximas e CV de pacientes com DPOC.
Realizamos um estudo transversal e randomizado em relação à sequência de início da avaliação (com ou sem HME) que incluiu 16 pacientes com DPOC em tratamento no setor de reabilitação cardiopulmonar e metabólica de uma clínica-escola. O valor médio e a dispersão do VEF1 nesses pacientes foram de 36,01 ± 10,56% do valor previsto e o valor médio e a dispersão da relação VEF1/CVF foram de 54,29 ± 10,01% do previsto. O tamanho da amostra foi por conveniência, o que justifica um número reduzido de pacientes, podendo ser uma limitação do estudo. O presente estudo foi aprovado pelo Comitê de ética em Pesquisa do Centro Universitário São Camilo (parecer no. 2.075.696). Os critérios de inclusão foram ter diagnóstico de DPOC confirmado por espirometria, não ter apresentado nenhuma exacerbação nos últimos seis meses, ter qualquer idade ou sexo e ter assinado o termo de consentimento livre e esclarecido. Os critérios de exclusão foram ter sido submetido à cirurgia torácica ou abdominal recente ou apresentar deformidades faciais, alterações cognitivas, miopatias ou problemas agudos de ouvido médio.
A avaliação de CV, PImáx e PEmáx foi feita com e sem o HME (filtro Bacteriológico Lumiar; Besmed Health Business Corp., New Taipei City, Taiwan), que é indicado para filtrar material do ar ambiente e/ou gases, reduzindo o risco de contaminação cruzada. A membrana do filtro apresenta alta eficiência de filtração bacteriana (> 99,99%). O HME foi posicionado entre o bocal e os equipamentos. Foram realizadas três medidas para cada variável estudada, e o maior valor foi considerado para a análise e então comparado com o valor obtido sem o HME no mesmo paciente. O ventilômetro usado foi Ferraris Mark 8 (Ferraris Respiratory Europe, Hertford, Reino Unido) e o manovacuômetro foi o Ger-Ar (Ger-Ar-SP Com. Equip. Ltda., São Paulo, Brasil).
Os dados numéricos apresentados foram expressos em média e desvio-padrão. Os dados foram testados para a normalidade com o teste de Shapiro-Wilk. A comparação entre os grupos que foram avaliados sem (convencional) e com a utilização do HME nas avaliações da CV, PImáx e PEmáx foi realizada pelo teste t pareado. Foi utilizado o pacote estatístico SigmaStat, versão 11.0 (Systat Software, Inc., San Jose, CA, EUA) e estabeleceu-se para fins de significância estatística o valor de p < 0,05.
Foram selecionados 16 pacientes com diagnóstico de DPOC, sendo 11 do sexo masculino. A média de idade foi de 69,9 ± 7,7 anos, a de peso foi de 66,0 ± 15,3 kg, a de altura foi de 1,62 ± 0,11 m, e a de índice de massa corpórea foi de 24,84 ± 5,04 kg/m2.
Na comparação entre o método convencional e com o uso do HME, não houve diferenças significativas na PImáx (−66,5 ± 6,5 cmH2O vs. −63,8 ± 5,5 cmH2O; p = 0,45), PEmáx (74,4 ± 5,4 cmH2O vs. 73,4 ± 6,4 cmH2O; p = 0,61) e CV (2.338,1 ± 211,5 mL vs. 2.350,0 ± 220,5 mL; p = 0,58).
Concluímos que o uso do HME não modifica as pressões respiratórias máximas e a CV em pacientes com DPOC.
REFERÊNCIAS1. Kim NS, Seo JH, Ko MH, Park SH, Kang SW, Won YH. Respiratory Muscle Strength in Patients With Chronic Obstructive Pulmonary Disease. Ann Rehabil Med. 2017;41(4):659-666. https://doi.org/10.5535/arm.2017.41.4.659
2. American Thoracic Society/European Respiratory Society. ATS/ERS Statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002;166(4):518-624. https://doi.org/10.1164/rccm.166.4.518
3. Craven ED, Steger KA, La Force FM. Pneumonia. In: Bennett JV, Brachman PS, editors. Hospital Infections. Philadelphia: Lippincott-Raven; 1998. p 487-511.
4. Thomachot L, Violet R, Arnaud S, Barberon B, Michael-Nguyen A, Martin C. Do the components of heat and moisture exchanger filters affect their humidifying efficacy and the incidence of nosocomial pneumonia? Crit Care Med. 1999;27(5):923-8. https://doi.org/10.1097/00003246-199905000-00026
5. Lucato JJ, Nogueira da Cunha TM, Rocha SS, Palmieri de Carvalho FM, Botega DC, Torquato JA, et al. Influence of heat and moisture exchanger use on measurements performed with manovacuometer and respirometer in healthy adults. Multidiscip Respir Med. 2015;11:1. https://doi.org/10.1186/s40248-015-0037-9
6. Morgan-Hughes NJ, Mills GH, Northwood D. Air flow resistance of three heat and moisture exchanging filter designs under wet conditions: implications for patient safety. Br J Anaesth. 2001;87(2):289-91. https://doi.org/10.1093/bja/87.2.289