ABSTRACT
Objective: Minimally invasive repair of pectus excavatum (MIRPE) is a surgical treatment for PE. During the procedure, a specialized introducer is used to tunnel across the mediastinum for thoracoscopic insertion of a metal bar. There have been reported cases of cardiac perforation during this risky step. The large introducer can be a dangerous lever in unskilled hands. We set out to determine the safety and feasibility of using regular instruments (i.e., not relying on special devices or tools) to create the retrosternal tunnel during MIRPE. Methods: This was a preliminary study of MIRPE with regular instruments (MIRPERI), involving 28 patients with PE. We recorded basic patient demographics, chest measurements, and surgical details, as well as intraoperative and postoperative complications. Results: Patients undergoing MIRPERI had Haller index values ranging from 2.58 to 5.56. No intraoperative complications occurred. Postoperative complications included nausea/vomiting in 8 patients, pruritus in 2, and dizziness in 2, as well as atelectasis, pneumothorax with thoracic drainage, pleural effusion, and dyspnea in 1 patient each. Conclusions: In this preliminary study, the rate of complications associated with MIRPERI was comparable to that reported in the literature for MIRPE. The MIRPERI approach has the potential to improve the safety of PE repair, particularly for surgeons that do not have access to certain special instruments or have not been trained in their use.
Keywords:
Funnel chest; Heart injuries; Thoracic wall; Intraoperative complications; Minimally invasive surgical procedures.
RESUMO
Objetivo: O minimally invasive repair of pectus excavatum (MIRPE, reparo minimamente invasivo do pectus excavatum) é um tratamento cirúrgico do PE. Durante o procedimento, utiliza-se um introdutor específico a fim de criar um túnel mediastinal para a colocação toracoscópica de uma barra metálica. Já houve casos relatados de perfuração cardíaca durante essa etapa arriscada. O introdutor grande pode ser uma perigosa alavanca em mãos inábeis. Propusemo-nos a determinar a segurança e viabilidade do uso de instrumentos comuns (isto é, sem contar com dispositivos ou ferramentas especiais) para criar o túnel retroesternal durante o MIRPE. Métodos: Estudo preliminar sobre o MIRPE with regular instruments (MIRPERI, MIRPE com instrumentos comuns), envolvendo 28 pacientes com PE. Foram registrados dados demográficos básicos dos pacientes, medições torácicas e detalhes cirúrgicos, bem como complicações intra e pós-operatórias. Resultados: Os pacientes submetidos ao MIRPERI apresentavam índice de Haller entre 2,58 e 5,56. Não ocorreram complicações intraoperatórias. As complicações pós-operatórias incluíram náusea/vômito em 8 pacientes, prurido em 2 e tontura em 2, bem como atelectasia, pneumotórax com drenagem torácica, derrame pleural e dispneia em 1 paciente cada. Conclusões: Neste estudo preliminar, a taxa de complicações associadas ao MIRPERI foi comparável à relatada na literatura para o MIRPE. A abordagem de MIRPERI tem o potencial de melhorar a segurança do reparo do PE, particularmente para cirurgiões que não têm acesso a certos instrumentos especiais ou não foram treinados para utilizá-los.
Palavras-chave:
Tórax em funil; Traumatismos cardíacos; Parede torácica; Complicações intraoperatórias; Procedimentos cirúrgicos minimamente invasivos.
INTRODUÇÃOO minimally invasive repair of pectus excavatum (MIRPE, reparo minimamente invasivo do pectus excavatum) foi realizado pela primeira vez em 1987 e apresentado à Associação Americana de Cirurgia Pediátrica em 1997. No procedimento, são utilizadas ferramentas específicas de MIRPE a fim de criar um túnel retroesternal para a colocação de uma ou mais barras metálicas para elevar o esterno. As barras metálicas permanecem no tórax até serem retiradas vários anos mais tarde.(1) Essa técnica rapidamente ganhou popularidade como alternativa à técnica convencional de reparo aberto, e o número de pacientes que se apresentam para correção cirúrgica do PE aumentou exponencialmente. Embora não seja isento de complicações, o MIRPE atualmente é considerado o tratamento padrão para o manejo do PE.(2)
Embora as complicações mais comuns do MIRPE sejam deslocamento da barra, infecção e pneumotórax, também foram relatadas complicações potencialmente fatais.(3,4) A etapa mais arriscada do procedimento, responsável por essas complicações, é a dissecção do mediastino para a criação do túnel. Essa etapa foi relacionada a muitos casos de lesão cardíaca com necessidade de toracotomia ou até resultando em morte.(5,6)
Para melhorar a segurança durante a dissecção mediastinal, várias modificações técnicas foram propostas. Por exemplo, relata-se que a toracoscopia é utilizada na maioria (83,7%) dos casos.(7) No entanto, mesmo com a dissecção do túnel retroesternal guiada por toracoscopia, foram descritos casos de perfuração cardíaca e laceração pericárdica. Portanto, o potencial para lesão cardíaca permanece apesar da visualização direta do pericárdio.(8,9) Uma revisão sistemática da literatura sobre complicações potencialmente fatais do MIRPE, publicada recentemente, mostrou que houve 12 casos publicados e 15 casos não relatados de lesões cardíacas, resultando em 9 mortes.(10) Esses números provavelmente estão subestimados.
A dissecção mediastinal é perigosa principalmente em razão de dois aspectos incompatíveis. O introdutor pectus - uma ferramenta exclusiva desenvolvida para a criação do túnel - é um instrumento muito longo (58,6 cm) que pode se tornar uma alavanca perigosa em mãos inábeis. Ao mesmo tempo, a região retrosternal, normalmente um espaço anatômico estreito, é ainda mais estreita em indivíduos com PE, em razão do desvio dorsal do esterno. Dada essa dificuldade, o objetivo do presente estudo foi avaliar a dissecção do túnel retroesternal em uma série de casos de pacientes submetidos ao MIRPE sem o uso do introdutor pectus. Em vez disso, optamos pelo uso de um instrumento cirúrgico comum, uma pinça Crawford. Referimo-nos a essa técnica como MIRPE with regular instruments (MIRPERI, MIRPE com instrumentos comuns).
MÉTODOSEntre março de 2014 e agosto de 2016, 31 pacientes com PE foram incluídos em uma série prospectiva de casos concebida para avaliar a segurança e eficácia do MIRPERI. O estudo foi realizado no Departamento de Cirurgia Torácica do Instituto do Coração do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo. O estudo foi aprovado pelo Comitê de Ética em Pesquisa do Hospital das Clínicas sob o registro nº UIN 2545, e todos os pacientes participantes assinaram um termo de consentimento livre e esclarecido.
Os critérios de inclusão seguiram os aplicados em nosso serviço de MIRPE para incluir pacientes a partir dos 11 anos de idade. Embora não encorajemos o uso do MIRPE em pacientes maduros, não temos um limite máximo de idade específico, pois se trata de uma decisão intraoperatória: se a parede torácica for rígida demais, fazemos a conversão para técnica combinada (MIRPE e Ravitch). Foram excluídos pacientes com morfologia complexa (carinatum/excavatum), aqueles com doenças esqueléticas, disfunção da coagulação, doenças cutâneas que afetam a parede torácica ou angiopatias, e também gestantes e pacientes obesos, sendo que a obesidade foi definida como índice de massa corporal > 30 kg/m2.
A avaliação padronizada realizada para a seleção dos pacientes foi a mesma utilizada rotineiramente em nosso serviço para a identificação de candidatos para o tratamento cirúrgico do PE. Envolve história clínica, exame físico, testes laboratoriais (incluindo testes de função pulmonar), radiografias de tórax, avaliação cardíaca (eletrocardiografia e ecocardiografia) e tomografia computadorizada (TC) inicial de baixa dose do tórax. Antes da aquisição das imagens de TC, os pacientes foram instruídos a respirar normalmente. As imagens de TC de baixa dose foram então obtidas com os pacientes em pausa respiratória durante a inspiração tranquila. As seguintes medições foram realizadas a partir das imagens de TC adquiridas no ponto mais profundo da deformidade (Figura 1): distância sagital entre a face posterior do esterno e a coluna anterior; distância de lado a lado; distância sagital dos hemitórax direito e esquerdo; ângulo de rotação esternal; e distância sagital entre o esterno posterior na posição hipotética corrigida e a coluna anterior, menos a distância entre o esterno posterior na posição real e a coluna anterior. Com base nesses dados, foi possível calcular o índice de Haller, o índice de correção, o ângulo de rotação esternal (< 30° vs. ≥ 30°) e o índice de assimetria da parede torácica.(11-13)

Descrevemos anteriormente em detalhes a técnica de MIRPE que geralmente empregamos.(14,15) Para destacar as modificações que propomos, resumimos as principais etapas do procedimento. Os pacientes são intubados com sonda traqueal de lúmen único. O uso de ventilação com volumes mais baixos ou períodos mais curtos de apneia evita a necessidade de intubação com sonda de duplo lúmen. A pele é demarcada no ponto de depressão mais profunda na linha média e no ponto de articulação em cada hemitórax. Realiza-se uma incisão lateralmente aos pontos de articulação em cada hemitórax, e cria-se um túnel subcutâneo na direção dos pontos de articulação.
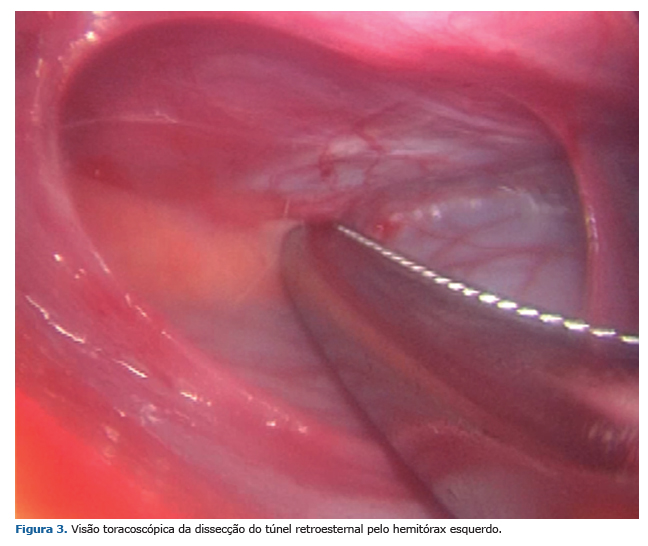
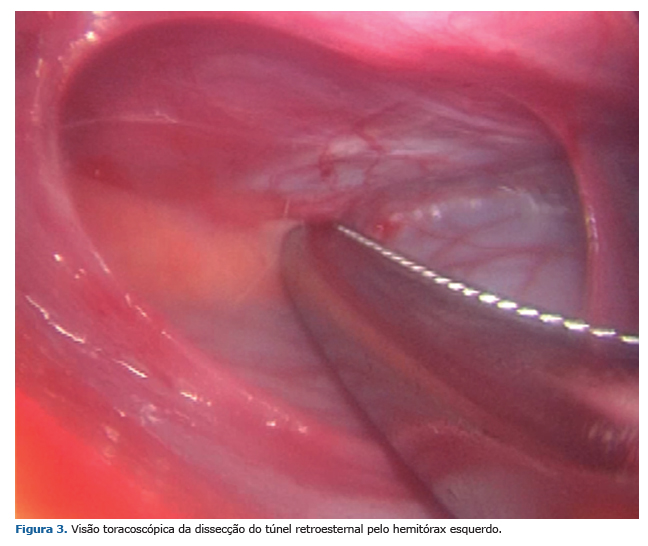
Embora alguns cirurgiões prefiram uma abordagem da direita para a esquerda, entramos primeiro na cavidade torácica esquerda com a câmera no ponto de articulação. Através da mesma incisão, introduz-se um trocarte rombo de 5,5 mm no espaço intercostal imediatamente abaixo do ponto de articulação, e transfere-se a câmera para esse espaço inferior. Introduz-se uma pinça Crawford de 24 cm no ponto de articulação, e, enquanto o toracoscópio e a pinça estão deslocando o pericárdio para baixo, disseca-se o túnel retroesternal com movimentos suaves (Figuras 2 e 3).

Assim que se cruza a linha média mediastinal, introduz-se o toracoscópio no lado direito e utiliza-se outra pinça Crawford para deslocar a almofada de gordura, evitando, assim, lesões nas principais artérias que conectam os vasos mamários internos e os vasos frênicos superiores anteriores que são encontrados em 12,5% das cavidades torácicas direitas e em 44,0% das cavidades torácicas esquerdas.(16)
Quando a pinça Crawford atravessa a almofada de gordura e atinge o hemitórax direito, coloca-se um dreno torácico 28 F no hemitórax direito através da incisão do ponto de articulação e traz-se o dreno de volta para o hemitórax esquerdo. O dreno torácico no túnel retroesternal representa um caminho seguro para guiar o introdutor pectus ou mesmo a barra metálica (Figura 4). O restante da cirurgia prossegue como de costume.

Para avaliar a segurança e eficácia da técnica de MIRPERI, foram registrados dados demográficos básicos dos pacientes, medições torácicas e detalhes cirúrgicos. Foram também avaliadas complicações intra e pós-operatórias.
RESULTADOSAs características básicas de todos os 31 pacientes avaliados para inclusão nesta série de casos estão resumidas na Tabela 1. Em três casos (pacientes 3, 4 e 7), o defeito era grave ou a parede torácica era rígida demais. Nesses casos, decidimos utilizar ressecção da cartilagem condral através de uma incisão na linha média antes de a barra metálica ser inserida abaixo do esterno (técnica combinada MIRPE + Ravitch). O túnel retroesternal foi confeccionado com abordagem bilateral combinada, e esses três casos foram excluídos de nossas análises. A Figura 5 demonstra um desses casos.

Dos 28 pacientes submetidos ao MIRPERI e incluídos na análise, 6 (21,4%) eram do sexo feminino. Nesta amostra de pacientes, a média de idade foi de 16 ± 3 anos (variação: 11-26 anos) e a média do índice de massa corporal foi de 18,2 ± 2,3 kg/m2 (variação, 14,0-22,3 kg/m2). A média do índice de Haller foi de 3,73 ± 0,87 (variação: 2,58-5,56) e foi semelhante entre os sexos masculino e feminino (3,80 ± 0,90 e 3,47 ± 0,71, respectivamente). Dos 28 pacientes, 22 (78,5%) receberam uma barra e 6 (21,4%) receberam duas barras. A média de duração da anestesia foi de 220 ± 38 min (variação: 150-305 min). Não ocorreram complicações intraoperatórias.
Em um caso, foi utilizado um dreno torácico em razão de pneumotórax no período pós-operatório. Um paciente desenvolveu derrame pleural que foi detectado por radiografia de tórax, embora o derrame tenha sido mínimo e tenha se resolvido espontaneamente. As outras complicações pós-operatórias foram náusea/vômito em 8 pacientes, prurido em 2, tontura em 2, atelectasia em 1 e dispneia em 1. Não foram observadas infecções do sítio cirúrgico. Não ocorreu nenhuma outra complicação grave. O tempo médio de internação foi de 5 ± 1 dias (variação, 3-7 dias).
DISCUSSÃONeste estudo, avaliamos a segurança e viabilidade do MIRPERI, uma versão levemente modificada do MIRPE na qual instrumentos comuns são utilizados para a dissecção do túnel retroesternal. Em nossa amostra de 28 pacientes, as taxas de complicações foram comparáveis às relatadas na literatura para o MIRPE,(4) e não houve complicações intra ou pós-operatórias graves.
A proposta de uso de instrumentos comuns para criar um túnel retroesternal para correção do PE pode soar como um retrocesso para alguns. Nos primeiros anos da correção do PE, o procedimento de Nuss era realizado com instrumental cirúrgico comum, embora naquela época a abordagem para a dissecção do túnel era pelo lado direito e não envolvia vídeo assistência. A evolução subsequente da técnica baseou-se no desenvolvimento de instrumentos exclusivos e no desenvolvimento mais recente de ferramentas ainda mais específicas. Portanto, é compreensível que o uso de instrumentos comuns seja considerado regressivo. No entanto, esse não é o caso, como se verá a seguir.
Embora seja inquestionável que o MIRPE com o procedimento de Nuss representa um grande avanço no tratamento cirúrgico do PE, também é preocupante que ainda se discuta a segurança do procedimento e que a real incidência de complicações graves e potencialmente fatais permaneça desconhecida.(10,17) A criação do túnel retrosternal, momento mais temido do procedimento, em razão do risco de lesão cardíaca, continua sendo fonte de grandes complicações. Além da dificuldade técnica de manusear o grande introdutor pectus dentro do estreito espaço mediastinal, há dois aspectos que podem complicar essa etapa, um anatômico e outro epidemiológico. Do ponto de vista anatômico, o coração geralmente se encontra deslocado para a esquerda no PE, fazendo com que a dissecção do túnel retroesternal do hemitórax direito para o esquerdo pareça ilógica. Do ponto de vista epidemiológico, exceto em centros com um grande número de casos de PE, o MIRPE não é um procedimento comum. Como resultado, um cirurgião torácico geral ou pediátrico pode não ter tido muitas oportunidades de se tornar hábil no uso do introdutor pectus.
Muitos cirurgiões propuseram modificações técnicas para reduzir o risco de lesão cardíaca em MIRPE. Essas incluem utilizar uma incisão subxifoide a fim de permitir a orientação dos dedos para a dissecção mediastinal(18,19) e iniciar a dissecção mediastinal com o introdutor em posição mais cranial e gradualmente avançar distalmente.(20) No entanto, o uso dessas técnicas resulta em cicatrizes adicionais na parede torácica anterior que podem ser consideradas inaceitáveis, já que a maioria dos pacientes com PE se submete a esse tipo de procedimento para melhora estética. Outro grupo de modificações inclui a dissecção do túnel retroesternal da esquerda para a direita e o uso de toracoscopia bilateral, bem como uma abordagem guiada por um videoscópio especialmente projetado. (15,21-23) Há um motivo para essas modificações. Como o coração encontra-se deslocado para a esquerda em pacientes com PE, iniciar a dissecção por esse lado sob visualização toracoscópica esquerda permite ao cirurgião empurrar o pericárdio para baixo e simultaneamente continuar a dissecção.
É claro que o que a maioria dos cirurgiões propõe para evitar lesão cardíaca é alguma técnica para promover a elevação esternal. Há pelo menos duas modificações técnicas que empregam instrumentos recentes e exclusivos para a elevação esternal, uma das quais ainda depende de uma incisão subxifoide adicional. (19,24) O principal problema dessas técnicas é que esses afastadores exclusivos geralmente estão disponíveis apenas para o grupo que os desenvolveu. Também houve sete relatos descrevendo manobras de elevação esternal que empregam dispositivos não exclusivos, incluindo o afastador Kent (Takasago Medical Co., Tóquio, Japão), o sistema afastador Rultract (Rultract Inc., OH, EUA) e o sistema Omni Crane (Primemed, Seul, Coreia do Sul). Embora algumas dependam de uma sequência complexa de etapas para agarrar o esterno antes de fixá-lo no afastador,(25) outras contam com o uso de um gancho fixado no esterno(26-28) ou mesmo com a colocação de suturas metálicas no esterno para completar a elevação.(29,30) Embora essas técnicas de elevação por grua sejam celebradas como a forma mais segura de facilitar a criação do túnel retroexternal, o ato de "agarrar" o esterno para elevação não é isento de complicações. Há um relato de perfuração pontual do coração por agulha. (31) Outra consideração importante é que, embora essas manobras para elevar o esterno envolvam o uso do que se poderia chamar de afastadores "tradicionais", esses dispositivos não estão disponíveis em todas as enfermarias cirúrgicas.
Como é difícil tornar-se hábil com o introdutor pectus e a maioria das manobras propostas para a criação do túnel retroesternal baseia-se em instrumentos nem sempre disponíveis, decidimos testar a viabilidade de utilizar apenas instrumentos comuns durante essa etapa cirúrgica. Embora os instrumentos toracoscópicos representem a escolha natural para esse propósito, a qual foi reservada como "plano B", optamos por utilizar instrumentos cirúrgicos verdadeiramente comuns. É por isso que escolhemos utilizar a pinça Crawford neste estudo. Obviamente, instrumentos mais longos, como as ferramentas endoscópicas, podem ser utilizados como alternativa.
Não estamos advogando contra o uso do introdutor pectus. Este estudo fornece dados preliminares sobre uma técnica substituta. Embora estejamos cientes de que essa sugestão pode parecer dispensável para cirurgiões que são especialistas no tratamento do PE, o número de complicações cardíacas relatadas na literatura durante o tratamento dessa condição benigna nos convenceu a considerar alternativas.
Este estudo apresenta algumas limitações. Do ponto de vista metodológico, seria mais apropriado avaliar dois grupos: um grupo controle de pacientes submetidos ao MIRPE tradicional (com o introdutor pectus) e outro grupo de pacientes submetidos ao MIRPERI. Como a taxa de complicações do MIRPE já está bem relatada na literatura e o reparo do PE não é um procedimento cirúrgico comum, escolhemos mostrar em uma série de casos que o procedimento pode ser realizado da maneira que propomos. Outra limitação é o pequeno número de pacientes. No entanto, considerando a relativa raridade do PE, acreditamos que 31 seja um número razoável de pacientes.
Em conclusão, nossos resultados mostram que é possível realizar a dissecção do túnel retroesternal com instrumentos comuns, mesmo em pacientes com índice de Haller chegando a 5,6 (paciente 11 do presente estudo, por exemplo). Essa técnica pode servir como alternativa para cirurgiões que se sentem inseguros quanto ao uso do introdutor pectus. Além disso, neste estudo preliminar sobre o MIRPERI, as taxas de complicações foram comparáveis às associadas ao MIRPE tradicional.(4) Acreditamos que a abordagem de MIRPERI, embora pareça um retrocesso, tem o potencial de melhorar a segurança do reparo do PE, particularmente para cirurgiões não acostumados com instrumentos pectus exclusivos ou os que não têm acesso a todos as ferramentas específicas necessárias para a realização do procedimento padrão. Estudos com amostras maiores de pacientes são necessários para confirmar nossos achados.
REFERÊNCIAS1. Nuss D, Kelly RE Jr, Croitoru DP, Katz ME. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg. 1998;33(4):545-52. https://doi.org/10.1016/S0022-3468(98)90314-1
2. Fallon SC, Slater BJ, Nuchtern JG, Cass DL, Kim ES, Lopez ME, et al. Complications related to the Nuss procedure: minimizing risk with operative technique. J Pediatr Surg. 2013;48(5):1044-8. https://doi.org/10.1016/j.jpedsurg.2013.02.025
3. Johnson WR, Fedor D, Singhal S. Systematic review of surgical treatment techniques for adult and pediatric patients with pectus excavatum. J Cardiothorac Surg. 2014;9:25 https://doi.org/10.1186/1749-8090-9-25
4. Kelly RE Jr, Mellins RB, Shamberger RC, Mitchell KK, Lawson ML, Oldham KT, et al. Multicenter study of pectus excavatum, final report: complications, static/exercise pulmonary function, and anatomic outcomes. J Am Coll Surg. 2013;217(6):1080-9. https://doi.org/10.1016/j.jamcollsurg.2013.06.019
5. Leonhardt J, Kübler JF, Feiter J, Ure BM, Petersen C. Complications of the minimally invasive repair of pectus excavatum. J Pediatr Surg. 2005;40(11):e7-e9. https://doi.org/10.1016/j.jpedsurg.2005.07.033
6. Gips H, Zaitsev K, Hiss J. Cardiac perforation by a pectus bar after surgical correction of pectus excavatum: case report and review of the literature. Pediatr Surg Int. 2008;24(5):617-20. https://doi.org/10.1007/s00383-007-2097-1
7. Becmeur F, Ferreira CG, Haecker FM, Schneider A, Lacreuse I. Pectus excavatum repair according to Nuss: is it safe to place a retrosternal bar by a transpleural approach, under thoracoscopic vision? J Laparoendosc Adv Surg Tech A. 2011;21(8):757-61. https://doi.org/10.1089/lap.2011.0035
8. Hebra A. Minimally invasive pectus surgery. Chest Surg Clin N Am. 2010;10(2):329-39, vii.
9. Umuroglu T, Bostanci K, Thomas DT, Yuksel M, Gogus FY. Perioperative anesthetic and surgical complications of the Nuss procedure. J Cardiothorac Vasc Anesth. 2013;27(3):436-40. https://doi.org/10.1053/j.jvca.2012.10.016
10. Hebra A, Kelly RE, Ferro MM, Yüksel M, Campos JRM, Nuss D. Life-threatening complications and mortality of minimally invasive pectus surgery. J Pediatr Surg. 2018;53(4):728-732. https://doi.org/10.1016/j.jpedsurg.2017.07.020
11. Haller JA Jr, Kramer SS, Lietman SA. Use of CT scans in selection of patients for pectus excavatum surgery: a preliminary report. J Pediatr Surg. 1987;22(10):904-6. https://doi.org/10.1016/S0022-3468(87)80585-7
12. Cartoski MJ, Nuss D, Goretsky MJ, Proud VK, Croitoru DP, Gustin T, et al. Classification of the dysmorphology of pectus excavatum. J Pediatr Surg. 2006;41(9):1573-81. https://doi.org/10.1016/j.jpedsurg.2006.05.055
13. St Peter SD, Juang D, Garey CL, Laituri CA, Ostlie DJ, Sharp RJ, et al. A novel measure for pectus excavatum: the correction index. J Pediatr Surg. 2011;46(12):2270-3. https://doi.org/10.1016/j.jpedsurg.2011.09.009
14. Tedde ML, Campos JR, Das-Neves-Pereira JC, Abrão FC, Jatene FB. The search for stability: bar displacement in three series of pectus excavatum patients treated with the Nuss technique. Clinics (Sao Paulo). 2011;66(10):1743-6. https://doi.org/10.1590/S1807-59322011001000012
15. Tedde ML, de Campos JR, Wihlm JM, Jatene FB. The Nuss procedure made safer: an effective and simple sternal elevation manoeuvre. Eur J Cardiothorac Surg. 2012;42(5):890-1. https://doi.org/10.1093/ejcts/ezs442
16. Nagasao T, Takayama M, Miyamoto J, Ding W, Jiang H. Anatomical study of the thorax for the safe performance of the Nuss procedure for pectus excavatum. Thorac Cardiovasc Surg. 2011;59(1):34-9. https://doi.org/10.1055/s-0030-1249922
17. Sacco-Casamassima MG, Goldstein SD, Gause CD, Karim O, Michailidou M, Stewart D, et al. Minimally invasive repair of pectus excavatum: analyzing contemporary practice in 50 ACS NSQIP-pediatric institutions. Pediatr Surg Int. 2015;31(5):493-9. https://doi.org/10.1007/s00383-015-3694-z
18. St Peter SD, Sharp SW, Ostlie DJ, Snyder CL, Holcomb GW 3rd, Sharp RJ. Use of a subxiphoid incision for pectus bar placement in the repair of pectus excavatum. J Pediatr Surg. 2010;45(6):1361-4. https://doi.org/10.1016/j.jpedsurg.2010.02.115
19. Johnson WR, Fedor D, Singhal S. A novel approach to eliminate cardiac perforation in the nuss procedure. Ann Thorac Surg. 2013;95(3):1109-11. https://doi.org/10.1016/j.athoracsur.2012.10.016
20. Ohno K, Nakamura T, Azuma T, Yamada H, Hayashi H, Masahata K. Modification of the Nuss procedure for pectus excavatum to prevent cardiac perforation. J Pediatr Surg. 2009;44(12):2426-30. https://doi.org/10.1016/j.jpedsurg.2009.09.006
21. Palmer B, Yedlin S, Kim S. Decreased risk of complications with bilateral thoracoscopy and left-to-right mediastinal dissection during minimally invasive repair of pectus excavatum. Eur J Pediatr Surg. 2007;17(2):81-3. https://doi.org/10.1055/s-2007-965012
22. Park HJ, Jeong JY, Jo WM, Shin JS, Lee IS, Kim KT, et al. Minimally invasive repair of pectus excavatum: a novel morphology-tailored, patient-specific approach. J Thorac Cardiovasc Surg. 2010;139(2):379-86. https://doi.org/10.1016/j.jtcvs.2009.09.003
23. Cheng YL, Lee SC, Huang TW, Wu CT. Efficacy and safety of modified bilateral thoracoscopy-assisted Nuss procedure in adult patients with pectus excavatum. Eur J Cardiothorac Surg. 2008;34(5):1057-61. https://doi.org/10.1016/j.ejcts.2008.07.068
24. Takagi S, Oyama T, Tomokazu N, Kinoshita K, Makino T, Ohjimi H. A new sternum elevator reduces severe complications during minimally invasive repair of the pectus excavatum. Pediatr Surg Int. 2012;28(6):623-6. https://doi.org/10.1007/s00383-012-3087-5
25. Kim D, Idowu O, Palmer B, Kim S. Anterior chest wall elevation using a T-fastener suture technique during a Nuss procedure. Ann Thorac Surg. 2014;98(2):734-6. https://doi.org/10.1016/j.athoracsur.2013.12.077
26. Rygl M, Vyhnanek M, Kucera A, Mixa V, Kyncl M, Snajdauf J. Technical innovation in minimally invasive repair of pectus excavatum. Pediatr Surg Int. 2014;30(1):113-7. https://doi.org/10.1007/s00383-013-3435-0
27. Jaroszewski DE, Johnson K, McMahon L, Notrica D. Sternal elevation before passing bars: a technique for improving visualization and facilitating minimally invasive pectus excavatum repair in adult patients. J Thorac Cardiovasc Surg. 2014;147(3):1093-5. https://doi.org/10.1016/j.jtcvs.2013.09.049
28. Takahashi T, Okazaki T, Yamataka A, Uchida E. Usefulness of Kent retractor and lifting hook for Nuss procedure. Pediatr Surg Int. 2015;31(11):1103-5. https://doi.org/10.1007/s00383-015-3764-2
29. Park HJ, Chung WJ, Lee IS, Kim KT. Mechanism of bar displacement and corresponding bar fixation techniques in minimally invasive repair of pectus excavatum. J Pediatr Surg. 2008;43(1):74-8. https://doi.org/10.1016/j.jpedsurg.2007.09.022
30. Yoon YS, Kim HK, Choi YS, Kim K, Shim YM, Kim J. A modified Nuss procedure for late adolescent and adult pectus excavatum. World J Surg. 2010;34(7):1475-80. https://doi.org/10.1007/s00268-010-0465-9
31. Jeong JY, Lee J. Use of needlescope and crane technique to avoid cardiac injury in Nuss procedure. Ann Thorac Surg. 2014;98(1):386-7. https://doi.org/10.1016/j.athoracsur.2013.11.054