ABSTRACT
Objective: To validate the Portuguese-language version of the STOP-Bang (acronym for Snoring, Tiredness, Observed apnea, high blood Pressure, Body mass index, Age, Neck circumference, and Gender) questionnaire, culturally adapted for use in Brazil, as a means of screening for obstructive sleep apnea (OSA) in adults. Methods: In this validation study, we enrolled patients ≥ 18 years of age, recruited between May of 2015 and August of 2016. All patients completed the STOP-Bang questionnaire and underwent overnight polysomnography. To evaluate the performance of the questionnaire, we used contingency tables and areas under the (receiver operating characteristic) curve (AUCs). Results: We included 456 patients. The mean age was 43.7 ± 12.5 years, and 291 (63.8%) of the patients were male. On the basis of the apnea-hypopnea index (AHI), we categorized OSA as mild/moderate/severe (any OSA; AHI ≥ 5 events/h), moderate/severe (AHI ≥ 15 events/h), or severe (AHI ≥ 30 events/h). The overall prevalence of OSA was 78.3%, compared with 52.0%, and 28.5% for moderate/severe and severe OSA, respectively. The most common score on the STOP-Bang questionnaire was 4 points (n = 106), followed by 3 points (n = 85) and 5 points (n = 82). An increase in the score was paralleled by a reduction in sensitivity with a corresponding increase in specificity for all AHI cut-off points. The AUCs obtained for the identification of any, moderate/severe, and severe OSA were: 0.743, 0.731, and 0.779, respectively. For any OSA, the score on the questionnaire (cut-off, ≥ 3 points) presented sensitivity, specificity, and accuracy of 83.5%, 45.5%, and 75.2%, respectively. Conclusions: The STOP-Bang questionnaire performed adequately for OSA screening, indicating that it could be used as an effective screening tool for the disorder.
Keywords:
Sleep apnea, obstructive/diagnosis; Polysomnography; Diagnostic techniques and procedures; Surveys and questionnaires.
RESUMO
Objetivo: Realizar a validação da versão brasileira do questionário STOP-Bang (acrônimo em inglês para Snoring, Tiredness, Observed apnea, high blood Pressure, Body mass index, Age, Neck circumference, and Gender) para a identificação de apneia obstrutiva do sono (AOS) em adultos. Métodos: Neste estudo de validação, foram incluídos pacientes com idade ≥ 18 anos, recrutados entre maio de 2015 e novembro de 2016. Todos os pacientes completaram o questionário STOP-Bang e foram submetidos a polissonografia de noite inteira. O índice de apneias e hipopneias (IAH) foi calculado. Foram utilizadas tabelas de contingência e a área sob a curva (ASC) ROC para avaliar o desempenho do questionário. Resultados: Foram incluídos 456 pacientes. A média de idade foi de 43,7 ± 12,5 anos, e 291 (63,8%) dos pacientes eram homens. Com base no IAH, a AOS foi classificada em leve/moderada/grave (AOS, independentemente da gravidade; IAH ≥ 5 eventos/h), cuja prevalência foi de 78,3%; moderada/grave (IAH ≥ 15 eventos/h), cuja prevalência foi de 52,0%; e grave (IAH ≥ 30 eventos/h), cuja prevalência foi de 28,5%. A pontuação mais frequentemente obtida no STOP-Bang foi 4 (n = 106), seguida de 3 (n = 85) e 5 (n = 82). O aumento da pontuação obtida no STOP-Bang (pontuação máxima: 8) resultou em redução da sensibilidade e aumento correspondente da especificidade em todos os pontos de corte do IAH (≥ 5, ≥ 15 e ≥ 30 eventos/h). A ASC para a identificação de AOS, AOS moderada/grave e AOS grave foi de 0,743, 0,731 e 0,779, respectivamente. Para a identificação de AOS, a pontuação no STOP-Bang (valor de corte ≥ 3) apresentou sensibilidade de 83,5%, especificidade de 45,5% e acurácia de 75,2%. Conclusões: O questionário STOP-Bang mostrou-se adequado para identificar AOS e pode ser uma ferramenta eficaz para o diagnóstico do transtorno.
Palavras-chave:
Apneia obstrutiva do sono/diagnóstico; Polissonografia; Técnicas e procedimentos diagnósticos; Inquéritos e questionários.
INTRODUÇÃOA apneia obstrutiva do sono (AOS) é o transtorno do sono mais comum e um grande problema de saúde pública, que afeta 2-4% da população adulta.(1,2) No entanto, em virtude do envelhecimento da população(3) e da epidemia de obesidade,(4) é possível que a prevalência da AOS seja maior do que já se relatou.(5-7) Os sinais, sintomas e consequências da AOS são resultado direto dos distúrbios relacionados com o colapso repetitivo das vias aéreas superiores(8): fragmentação do sono, hipoxemia, hipercapnia, oscilações acentuadas da pressão intratorácica e aumento da atividade simpática. Se não for tratada, a AOS limita a capacidade de realizar atividades cotidianas, piora a qualidade de vida, compromete a segurança pessoal e diminui a produtividade no trabalho, além de aumentar os gastos com cuidados de saúde.(3,4)
O atual padrão ouro para o diagnóstico de AOS é a polissonografia de noite inteira em laboratório. No entanto, a AOS tornou-se tão prevalente que os laboratórios do sono disponíveis estão sobrecarregados. Os laboratórios do sono em todo o mundo têm longas listas de espera de pacientes com suspeita de AOS.(9) Para resolver esse problema, diversos questionários e modelos clínicos de avaliação foram elaborados para ajudar a identificar pacientes com suspeita de AOS.(10-16) A grande maioria desses modelos foi elaborada em outros países, e ainda não está claro se são reproduzíveis no Brasil. O uso de ferramentas práticas de avaliação provavelmente resultará em maior taxa de diagnóstico e redução dos custos. Isso é especialmente verdadeiro no caso de métodos diagnósticos portáteis em regiões com recursos limitados.
O questionário STOP-Bang (acrônimo em inglês para Snoring, Tiredness, Observed apnea, high blood Pressure, Body mass index, Age, Neck circumference, and Gender) e seu antecessor, o questionário STOP, foram originalmente elaborados e validados para uso em pacientes submetidos à cirurgia.(14) Tanto o STOP como o STOP-Bang são questionários autoaplicáveis e consistem em 4 e 8 perguntas do tipo sim/não, respectivamente. Quando se usou um valor de corte ≥ 3 pontos em uma amostra de pacientes submetidos a cirurgia, o questionário STOP-Bang apresentou as seguintes probabilidades condicionais de diagnóstico de AOS(14): sensibilidade de 83,6%, especificidade de 56,4%, valor preditivo positivo (VPP) de 81,0% e valor preditivo negativo (VPN) de 60,8%.
A população do Brasil inclui indivíduos de diversos grupos étnicos, raciais e sociais. Em virtude da miscigenação generalizada no país, pode ser útil determinar a validade e o desempenho do questionário STOP-Bang nesse cenário. Pelo que sabemos, nenhum estudo determinou a reprodutibilidade desse questionário no Brasil. O objetivo do presente estudo foi validar a versão em português do questionário STOP-Bang previamente adaptada para uso no Brasil(17) - doravante denominada questionário STOP-Bang - em pacientes com suspeita de AOS submetidos à polissonografia de noite inteira.
MÉTODOSSeleção de pacientesPacientes ambulatoriais consecutivos foram recrutados entre os encaminhados para polissonografia de noite inteira em dois laboratórios do sono no Brasil: um na cidade de Goiânia (no período decorrido de maio de 2015 a agosto de 2015, n = 229) e um na cidade do Rio de Janeiro (no período decorrido de outubro de 2016 a novembro de 2016, n = 227). O protocolo do estudo foi aprovado pelos Comitês de Ética em Pesquisa do Hospital Alberto Rassi, em Goiânia (Protocolo n. 752/14) e da Universidade Federal do Rio de Janeiro, no Rio de Janeiro (Protocolo n. 1.764.165). Todos os procedimentos foram realizados de acordo com a Declaração de Helsinque, e todos os pacientes participantes assinaram um termo de consentimento livre e esclarecido.
Todos os dados clínicos e polissonográficos foram coletados prospectivamente. Foram aplicados os seguintes critérios de inclusão: idade ≥ 18 anos; sem diagnóstico prévio de AOS e encaminhamento para polissonografia em laboratório do sono, independentemente do motivo. Foram excluídos os pacientes que haviam participado da adaptação cultural do questionário STOP-Bang,(17) bem como aqueles que não preencheram o questionário ou que o preencheram incorretamente e aqueles cuja polissonografia foi incompleta ou tecnicamente inadequada.
Aplicação do questionário STOP-BangDepois de assinar o termo de consentimento livre e esclarecido, os pacientes completaram o questionário STOP-Bang. As quatro primeiras perguntas - as que correspondem à porção "STOP" do questionário - foram respondidas pelos próprios pacientes. As respostas às perguntas correspondentes à porção "Bang" do questionário foram anotadas pelo pesquisador em um formulário padronizado. O peso corporal foi medido em quilogramas, e a altura foi medida em metros. O índice de massa corpórea (IMC) foi então calculado por meio da divisão do peso em quilogramas pela altura em metros quadrados (kg/m2). A circunferência do pescoço foi medida na altura da membrana cricotireoidea com uma fita métrica de 150 cm, cujas menores marcações estavam dispostas a 0,01 cm de distância umas das outras.
Estudos do sonoTodos os estudos do sono foram realizados em Goiânia, em um sistema de diagnóstico do sono Alice 5 (Philips Respironics, Murrysville, PA, EUA) ou no Rio de Janeiro, em um sistema digital EMBLA S7000 (Embla Systems Inc., Broomfield, CO, EUA). Foram realizados os seguintes procedimentos: eletroencefalografia; eletro-oculografia esquerda e direita; eletromiografia dos músculos submental e tibial anterior; detecção de roncos; monitoramento do fluxo aéreo nasal (com cânula nasal); avaliação do esforço respiratório (por meio de tiras torácicas e abdominais); oximetria de pulso; eletrocardiografia; monitoramento da posição do corpo; e captura de vídeo digital. Pontos foram manualmente atribuídos aos registros polissonográficos, que foram interpretados de acordo com as diretrizes existentes,(18) cuja definição de apneia é uma redução ≥ 90% do fluxo aéreo durante ≥ 10 s e cuja definição de hipopneia é uma redução ≥ 30% do fluxo aéreo durante ≥ 10 s, acompanhada de dessaturação ≥ 3% ou despertar. O índice de apneias e hipopneias (IAH) foi calculado por meio da determinação do total de eventos de apneia e hipopneia por hora de sono. O diagnóstico de AOS baseou-se em um IAH ≥ 5 eventos/h. A gravidade da AOS foi classificada da seguinte forma: leve/moderada/grave (AOS, independentemente da gravidade; IAH ≥ 5 eventos/h); moderada/grave (IAH ≥ 15 eventos/h); grave (IAH ≥ 30 eventos/h). Em ambos os laboratórios do sono, os médicos que realizaram os exames polissonográficos não estavam cientes da pontuação obtida no STOP-Bang.
Análise estatísticaA análise estatística foi realizada por meio do programa IBM SPSS Statistics, versão 23.0 para Windows (IBM Corporation, Armonk, NY, EUA). As variáveis contínuas estão expressas em forma de média e desvio-padrão, ao passo que as variáveis categóricas (dicotômicas) estão expressas em forma de frequência absoluta e relativa. Os grupos foram comparados por meio do teste do qui-quadrado (para variáveis dicotômicas), do teste t de Student e de ANOVA de uma via (para variáveis contínuas distribuídas normalmente) ou do teste U de Mann-Whitney e do teste de Kruskal-Wallis (para variáveis contínuas distribuídas não normalmente). As correlações foram avaliadas por meio da determinação do coeficiente de correlação de Spearman (rs). As curvas ROC e a área sob a curva (ASC) ROC foram avaliadas nos três limites do IAH (5 eventos/h, 15 eventos/h e 30 eventos/h). Testes multivariados foram usados para calcular as odds ratios e seus respectivos intervalos de confiança de 95%. Por meio de tabelas de contingência 2 × 2, calculamos as seguintes probabilidades condicionais: sensibilidade, especificidade, VPP, VPN, acurácia, razões de verossimilhança e odds ratios. A probabilidade pós-teste de cada pontuação obtida no STOP-Bang foi calculada por meio de regressão logística. Todos os testes estatísticos foram bilaterais, e valores de p < 0,05 foram considerados estatisticamente significativos.
RESULTADOSForam encaminhados para polissonografia diagnóstica 522 pacientes. Dos 522 pacientes, 66 (12,6%) foram excluídos, pelos seguintes motivos: 50 porque a polissonografia foi tecnicamente inadequada; 11 porque o questionário STOP-Bang não foi preenchido corretamente e 5 porque já haviam participado da adaptação cultural do questionário. Portanto, a população final do estudo compreendeu 456 pacientes, em duas amostras independentes: uma proveniente do Rio de Janeiro (n = 229) e outra de Goiânia (n = 227). Como se pode ver na Tabela 1, 63,8% dos pacientes eram do sexo masculino, a média de idade foi de 43,7 ± 12,5 anos, a média do IMC foi de 32,1 ± 7,8 kg/m2 e a média da circunferência do pescoço foi de 40,8 ± 4,3 cm. Houve diferenças estatisticamente significativas entre os pacientes com e sem AOS quanto a todas as variáveis contínuas (idade, IMC e circunferência do pescoço); os pacientes com AOS (IAH ≥ 5 eventos/h) eram mais velhos (p < 0,001) e apresentavam maior IMC e circunferência do pescoço (p = 0,001 e p < 0,001, respectivamente). Houve diferença estatisticamente significativa entre os pacientes com e sem AOS quanto a seis dos oito itens do questionário STOP-Bang; as exceções foram os itens "fatigado" (p = 0,730) e "obesidade", isto é, IMC > 35 kg/m2 (p = 0,705). Em comparação com os pacientes sem AOS, aqueles com AOS apresentaram maior probabilidade de roncar (p = 0,002), apresentar apneia (p < 0,001), ter hipertensão (p < 0,001), ter mais de 50 anos de idade (p = 0,011), ter circunferência do pescoço > 40 cm (p < 0,001) e ser do sexo masculino (p < 0,001). Entre os pacientes com AOS grave (IAH ≥ 30 eventos/h), a média de idade foi de 45,9 ± 12,8 anos, a média do IMC foi de 33,5 ± 7,9 kg/m2 e a média da circunferência do pescoço foi de 43,1 ± 4,2 cm.
A prevalência global de AOS foi de 78,3%, ao passo que a prevalência de AOS moderada/grave foi de 52,0% e a de AOS grave foi de 28,5%. Além disso, a prevalência global de AOS foi maior nos homens que nas mulheres (84,5% vs. 67,3%), assim como o foi a prevalência de AOS moderada/grave (60,1% vs. 37,6%) e de AOS grave (36,4% vs. 14,5%); as diferenças foram estatisticamente significativas (p < 0,001 para todas). Isso sugere que o sexo masculino influencia a ocorrência de AOS.

A Tabela 2 mostra as odds ratios ajustadas para todos os oito itens do questionário STOP-Bang em relação à gravidade da AOS. Apenas três itens foram preditores independentes em todos os três limites do IAH: apneia observada, idade e circunferência do pescoço. Por outro lado, o item "fatigado" não foi um preditor independente em nenhum limite do IAH (p = 0,912 para AOS, p = 0,397 para AOS moderada/grave e p = 0,097 para AOS grave). O melhor preditor de AOS moderada/grave foi a circunferência do pescoço (OR ajustada: 2,347; IC95%: 1,445-3,816), seguido de idade (OR ajustada: 2,132; IC95%: 1,308-3,472) e apneia observada (OR ajustada: 1,897; IC95%: 1,233-2,923).
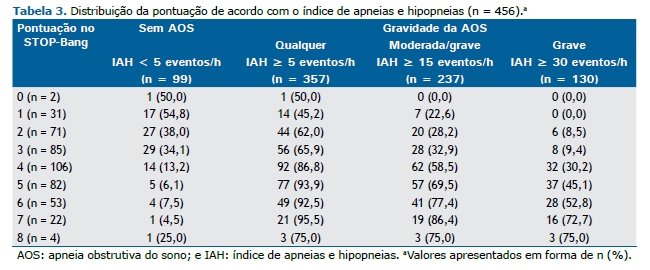
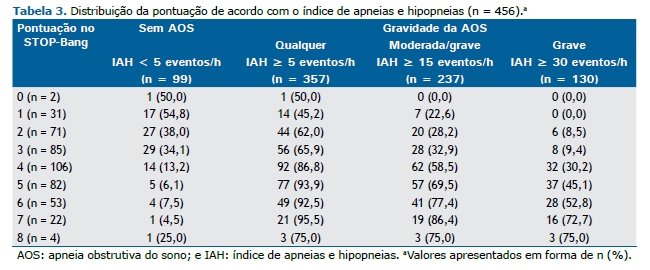
A Tabela 3 mostra a distribuição dos parâmetros de acordo com a gravidade da AOS. A pontuação mais frequentemente obtida no STOP-Bang foi 4 (em 106 pacientes), seguida de 3 (em 85) e 5 (em 82). Por meio do valor de corte de 3 pontos no questionário STOP-Bang, 34,1% dos pacientes foram classificados em pacientes sem AOS (IAH < 5 eventos/h) e 9,4% foram classificados em pacientes com AOS grave (IAH ≥ 30 eventos/h). A média da pontuação no STOP-Bang foi de 3,8 ± 1,6 na população do estudo como um todo e foi significativamente menor nas mulheres que nos homens (2,8 ± 1,3 pontos vs. 4,4 ± 1,4 pontos; p < 0,001). Além disso, a média da pontuação no STOP-Bang aumentou significativamente em paralelo com o aumento da gravidade da AOS, de 2,8 ± 1,4 pontos nos pacientes sem AOS para 4,1 ± 1,5 pontos naqueles com AOS, independentemente da gravidade, 4,5 ± 1,5 pontos naqueles com AOS moderada/grave e 5,0 ± 1,3 pontos naqueles com AOS grave; o valor de p da tendência foi < 0,001.

A Tabela 4 mostra o desempenho do questionário STOP-Bang. Como se pode ver na tabela, a pontuação de corte no STOP-Bang (≥ 3 pontos) apresentou as seguintes probabilidades condicionais de identificação de AOS, independentemente da gravidade: sensibilidade de 83,5%, especificidade de 45,5%, VPP de 84,7 %, VPN de 43,3% e acurácia de 75,2%. Para a identificação de AOS moderada/grave, a mesma pontuação de corte no STOP-Bang apresentou sensibilidade de 88,6%, especificidade de 35,2%, VPP de 59,7%, VPN de 74,0% e acurácia de 62,9%; para a identificação de AOS grave, apresentou sensibilidade de 95,4%, especificidade de 30,1%, VPP de 35,2%, VPN de 94,2% e acurácia de 48,7%. Houve correlação positiva entre a pontuação obtida no questionário STOP-Bang e o IAH (rs = 0,516; p < 0,001). De acordo com as curvas ROC (Figura 1), o questionário STOP-Bang apresentou as seguintes ASC: 0,743 (IC95%: 0,689-0,798) para o diagnóstico de AOS, independentemente da gravidade; 0,731 (IC95%: 0,685-0,777) para o diagnóstico de AOS moderada/grave; 0,779 (IC95%: 0,735-0,824) para o diagnóstico de AOS grave. A Tabela 5 resume a previsão de AOS, independentemente da gravidade, AOS moderada/grave e AOS grave em relação às diversas pontuações possíveis no questionário STOP-Bang. Para uma pontuação ≥ 3, a probabilidade pós-teste de AOS (independentemente da gravidade), AOS moderada/grave e AOS grave foi de 84,7%, 59,6% e 35,2%, respectivamente.

 DISCUSSÃO
DISCUSSÃONeste estudo prospectivo, o questionário STOP-Bang mostrou-se uma ferramenta promissora para a identificação de AOS em pacientes encaminhados para laboratórios do sono no Brasil. São vários os benefícios do questionário STOP-Bang: redução do risco de complicações peri e pós-operatórias, que muitas vezes não são diagnosticadas em pacientes com AOS submetidos à cirurgia(19); redução da ocorrência de comorbidades, minimizando assim os custos de cuidados de saúde relacionados com o transtorno; pode permitir um método diagnóstico portátil, o que pode ser crucial em regiões com recursos limitados, onde a polissonografia não está amplamente disponível. Além disso, o desempenho do questionário STOP-Bang foi bastante semelhante ao relatado em estudos anteriores a respeito dos questionários STOP e STOP-Bang(14,20-25): sensibilidade elevada e especificidade de baixa a moderada, o que pode ser crítico nas formas mais graves de AOS, resultando em diminuição da acurácia (isto é, da proporção de indivíduos avaliados corretamente). Esse aspecto de seu desempenho preditivo (a baixa especificidade) também já foi relatado em diversos estudos cujo objetivo foi traduzir, adaptar ou validar o questionário STOP-Bang.(21-25)
Nosso estudo mostrou alta prevalência de AOS em geral, além de alta prevalência de AOS moderada/grave e AOS grave. Isso poderia ser explicado pelo fato de que o estudo foi realizado em laboratórios do sono. Diferentemente de estudos realizados na comunidade, estudos realizados em laboratórios do sono relataram taxas de prevalência de AOS de 42-76%.(10) Nosso estudo, semelhantemente a estudos anteriores, demonstrou que a prevalência de AOS é maior em homens que em mulheres.(3,8,26-30) Além disso, os homens geralmente apresentam sintomas típicos, tais como ronco e apneia observada, ao passo que as mulheres são mais propensas a apresentar sintomas atípicos, tais como depressão, fadiga e insônia.(26-29) Há também diferenças entre os sexos quanto aos dados antropométricos e demográficos: os homens geralmente têm circunferência do pescoço maior que a das mulheres,(31) ao passo que as mulheres com AOS são geralmente mais velhas que os homens com AOS.(3) Além disso, o desempenho de um questionário para AOS pode variar amplamente, dependendo da população estudada e do ponto de corte do IAH usado para o diagnóstico de AOS.(10,11) O questionário de Berlim, por exemplo, foi inicialmente criado para uso na atenção primária à saúde,(13) e, portanto, é possível que seu desempenho seja melhor nesse cenário do que em laboratórios do sono.(32) Por outro lado, o questionário STOP-Bang foi inicialmente criado para uso em pacientes submetidos à cirurgia.(14) Embora tenha sido amplamente validado como ferramenta de avaliação,(20) o questionário STOP-Bang foi considerado inadequado como meio de confirmar a presença de AOS significativa em pacientes em uma instituição da Veterans Administration nos Estados Unidos, possivelmente em virtude da baixa especificidade (4,9%) obtida naquele estudo.(33)
O STOP-Bang é um instrumento de avaliação com alta sensibilidade, que aumenta em proporção ao aumento do limite do IAH usado (de 5 eventos/h a 30 eventos/h). (14) Por outro lado, apresenta especificidade de baixa a moderada, o que reduz sua acurácia. Como dá prioridade à sensibilidade em vez da especificidade, o questionário STOP-Bang classifica um grande número de pacientes em pacientes de alto risco, aumentando assim a taxa de resultados positivos falsos. Consequentemente, o questionário STOP-Bang não é suficiente para descartar a necessidade de estudo do sono em todos os pacientes. Outra característica importante do instrumento é que o aumento da pontuação de corte (pontuação máxima: 8) resulta em aumento da probabilidade pós-teste.(34-36) Infelizmente, nosso estudo não conseguiu mostrar um aumento linear da probabilidade pós-teste com o aumento da pontuação no STOP-Bang, exceto nos pacientes com AOS grave, nos quais tal aumento foi observado com todas as pontuações.
Um estudo anterior avaliou quatro ferramentas para a identificação de AOS(37): a four-variable screening tool, o questionário STOP, o questionário STOP-Bang e a Escala de Sonolência de Epworth. Para prever AOS moderada/grave, o questionário STOP-Bang apresentou a maior sensibilidade (87,0%), com ASC = 0,64, ao passo que a four-variable screening tool apresentou a maior especificidade (93,2%) e acurácia (79,4%). Achados semelhantes foram relatados em outro estudo, no qual foram comparados cinco questionários diferentes (o questionário STOP, o questionário STOP-Bang, o questionário de Berlim, a Escala de Sonolência de Epworth e a four-variable screening tool).(38) No estudo em questão, o questionário STOP-Bang apresentou a maior sensibilidade (97,6%) e a menor especificidade (12,7%) para a identificação de AOS moderada/grave.
O presente estudo tem algumas limitações que precisam ser mencionadas. O estudo incluiu pacientes encaminhados para o laboratório do sono, os quais são tipicamente pacientes pré-selecionados, o que poderia representar um viés de seleção. Além disso, não comparamos o desempenho do questionário STOP-Bang com o de outros instrumentos de avaliação validados, e, portanto, há necessidade de mais estudos, nos quais o STOP-Bang e essas ferramentas sejam comparados. Não obstante, nosso estudo foi realizado com uma amostra considerável de adultos, todos os quais foram submetidos à polissonografia de noite inteira, que é o padrão ouro para o diagnóstico de AOS. Outros pontos positivos foram o fato de que nosso estudo foi um estudo prospectivo, com análise manual dos resultados da polissonografia, e o fato de que os médicos envolvidos nos exames polissonográficos não tinham conhecimento prévio dos resultados do STOP-Bang.
Em suma, o questionário STOP-Bang teve bom desempenho na identificação de AOS e pode prever a gravidade do transtorno. A validação do questionário STOP-Bang promoverá seu uso como importante ferramenta de identificação de AOS em laboratórios do sono no Brasil. Como nosso estudo foi realizado em laboratórios do sono, são necessários mais estudos para validar o uso do questionário STOP-Bang em outros contextos (na atenção primária à saúde, por exemplo).
AGRADECIMENTOSOs autores gostariam de agradecer à Dra. Frances Chung sua bondade ao autorizar a validação do questionário STOP-Bang para uso no Brasil.
REFERÊNCIAS1. Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263-76.
2. Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230-5. https://doi.org/10.1056/NEJM199304293281704
3. Gabbay IE, Lavie P. Age- and gender-related characteristics of obstructive sleep apnea. Sleep Breath. 2012;16(2):453-60. https://doi.org/10.1007/s11325-011-0523-z
4. Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284-91. https://doi.org/10.1001/jama.2016.6458
5. Tufik S, Santos-Silva R, Taddei JA, Bittencourt LR. Obstructive sleep apnea syndrome in the Sao Paulo Epidemiologic Sleep Study. Sleep Med. 2010;11(5):441-6. https://doi.org/10.1016/j.sleep.2009.10.005
6. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006-14. https://doi.org/10.1093/aje/kws342
7. Heinzer R, Vat S, Marques-Vidal P, Marti-Soler H, Andries D, Tobback N, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015;3(4):310-8. https://doi.org/10.1016/S2213-2600(15)00043-0
8. Aurora RN, Collop NA, Jacobowitz O, Thomas SM, Quan SF, Aronsky AJ. Quality measures for the care of adult patients with obstructive sleep apnea. J Clin Sleep Med. 2015;11(3):357-83. https://doi.org/10.5664/jcsm.4556
9. Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep. 1997;20(9):705-6. https://doi.org/10.1093/sleep/20.9.705
10. Abrishami A, Khajehdehi A, Chung F. A systematic review of screening questionnaires for obstructive sleep apnea. Can J Anesth. 2010;57(5):423-38. https://doi.org/10.1007/s12630-010-9280-x
11. Ramachandran SK, Josephs LA. A meta-analysis of clinical screening tests for obstructive sleep apnea. Anesthesiology. 2009;110(4):928-39. https://doi.org/10.1097/ALN.0b013e31819c47b6
12. Flemons WW, Whitelaw WA, Brant R, Remmers JE. Likelihood ratios for a sleep apnea clinical prediction rule. Am J Respir Crit Care Med. 1994;150(5 Pt 1):1279-85. https://doi.org/10.1164/ajrccm.150.5.7952553
13. Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131(7):485-91. https://doi.org/10.7326/0003-4819-131-7-199910050-00002
14. Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108(5):812-21. https://doi.org/10.1097/ALN.0b013e31816d83e4
15. Takegami M, Hayashino Y, Chin K, Sokejima S, Kadotani H, Akashiba T, et al. Simple four-variable screening tool for identification of patients with sleep-disordered breathing. Sleep. 2009;32(7):939-48.
16. Marti-Soler H, Hirotsu C, Marques-Vidal P, Vollenweider P, Waeber G, Preisig M, et al. The NoSAS score for screening of sleep-disordered breathing: a derivation and validation study. Lancet Respir Med. 2016;4(9):742-8. https://doi.org/10.1016/S2213-2600(16)30075-3
17. Fonseca LB, Silveira EA, Lima NM, Rabahi MF. STOP-Bang questionnaire: translation to Portuguese and cross-cultural adaptation for use in Brazil. J Bras Pneumol. 2016;42(4):266-72. https://doi.org/10.1590/s1806-37562015000000243
18. Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597-619.
19. Singh M, Liao P, Kobah S, Wijeysundera DN, Shapiro C, Chung F. Proportion of surgical patients with undiagnosed obstructive sleep apnoea. Br J Anaesth. 2013;110(4):629-36. https://doi.org/10.1093/bja/aes465
20. Nagappa M, Liao P, Wong J, Auckley D, Ramachandran SK, Memtsoudis S, et al. Validation of the STOP-Bang questionnaire as a screening tool for obstructive sleep apnea among different populations: a systematic review and meta-analysis. PLoS One. 2015;10(12):e0143697. https://doi.org/10.1371/journal.pone.0143697
21. Luo J, Huang R, Zhong X, Xiao Y, Zhou J. Value of STOP-Bang questionnaire in screening patients with obstructive sleep apnea hypopnea syndrome in sleep disordered breathing clinic. Chin Med J (Engl). 2014;127(10):1843-8.
22. Bille DJ, Bille-Hasselstrøm C, Petersen CG. Translation and validation of the Stop-Bang Questionnaire for obstructive sleep apnoea into Danish. Dan Med J. 2015;62(12):A5158.
23. Sadeghniiat-Haghighi K, Montazeri A, Khajeh-Mehrizi A, Ghajarzadeh M, Alemohammad ZB, Aminian O, et al. The STOP-BANG questionnaire: reliability and validity of the Persian version in sleep clinic population. Qual Life Res. 2015;24(8):2025-30. https://doi.org/10.1007/s11136-015-0923-9
24. Alhouqani S, Al Manhali M, Al Essa A, Al-Houqani M. Evaluation of the Arabic version of STOP-Bang questionnaire as a screening tool for obstructive sleep apnea. Sleep Breath. 2015;19(4):1235-40. https://doi.org/10.1007/s11325-015-1150-x
25. Reis R, Teixeira F, Martins V, Sousa L, Batata L, Santos C, et al. Validation of a Portuguese version of the STOP-Bang questionnaire as a screening tool for obstructive sleep apnea: Analysis in a sleep clinic. Rev Port Pneumol (2006). 2015;21(2):61-8. https://doi.org/10.1016/j.rppnen.2014.04.009
26. Quintana-Gallego E, Carmona-Bernal C, Capote F, Sánchez-Armengol A, Botebol-Benhamou G, Polo-Padillo J, et al. Gender differences in obstructive sleep apnea syndrome: a clinical study of 1166 patients. Respir Med. 2004;98(10):984-9. https://doi.org/10.1016/j.rmed.2004.03.002
27. Basoglu OK, Tasbakan MS. Gender differences in clinical and polysomnographic features of obstructive sleep apnea: a clinical study of 2827 patients. Sleep Breath. 2017 Feb 14 [Epub ahead of print] https://doi.org/10.1007/s11325-017-1482-9
28. Valipour A, Lothaller H, Rauscher H, Zwick H, Burghuber OC, Lavie P. Gender-related differences in symptoms of patients with suspected breathing disorders in sleep: a clinical population study using the sleep disorders questionnaire. Sleep. 2007;30(3):312-9. https://doi.org/10.1093/sleep/30.3.312
29. Shah N, Hanna DB, Teng Y, Sotres-Alvarez D, Hall M, Loredo JS, et al. Sex-specific prediction models for sleep apnea from the Hispanic Community Health Study/Study of Latinos. Chest. 2016;149(6):1409-18. https://doi.org/10.1016/j.chest.2016.01.013
30. Duarte RL, Magalhães-da-Silveira FJ. Factors predictive of obstructive sleep apnea in patients undergoing pre-operative evaluation for bariatric surgery and referred to a sleep laboratory for polysomnography. J Bras Pneumol. 2015;41(5):440-8. https://doi.org/10.1590/S1806-37132015000000027
31. Dancey DR, Hanly PJ, Soong C, Lee B, Shepard J Jr, Hoffstein V. Gender differences in sleep apnea: the role of neck circumference. Chest 2003;123(5):1544-50. https://doi.org/10.1378/chest.123.5.1544
32. Ahmadi N, Chung SA, Gibbs A, Shapiro CM. The Berlin questionnaire for sleep apnea in a sleep clinic population: relationship to polysomnographic measurement of respiratory disturbance. Sleep Breath. 2008;12(1):39-45. https://doi.org/10.1007/s11325-007-0125-y
33. Kunisaki KM, Brown KE, Fabbrini AE, Wetherbee EE, Rector TS. STOP-BANG questionnaire performance in a Veterans Affairs unattended sleep study program. Ann Am Thorac Soc. 2014;11(2):192-7. https://doi.org/10.1513/AnnalsATS.201305-134OC
34. Chung F, Subramanyam R, Liao P, Sasaki E, Shapiro C, Sun Y. High STOP-Bang score indicates a high probability of obstructive sleep apnoea. Br J Anaesth. 2012;108(5):768-75. https://doi.org/10.1093/bja/aes022
35. Chung F, Yang Y, Liao P. Predictive performance of the STOP-Bang score for identifying obstructive sleep apnea in obese patients. Obes Surg. 2013;23(12):2050-7. https://doi.org/10.1007/s11695-013-1006-z
36. Farney RJ, Walker BS, Farney RM, Snow GL, Walker JM. The STOP-Bang equivalent model and prediction of severity of obstructive sleep apnea: relation to polysomnographic measurements of the apnea/hypopnea index. J Clin Sleep Med. 2011;7(5):459-65B. https://doi.org/10.5664/jcsm.1306
37. Silva GE, Vana KD, Goodwin JL, Sherrill DL, Quan SF. Identification of patients with sleep disordered breathing: comparing the four-variable screening tool, STOP, STOP-Bang, and Epworth Sleepiness Scales. J Clin Sleep Med. 2011;7(5):467-72. https://doi.org/10.5664/jcsm.1308
38. Pataka A, Daskalopoulou E, Kalamaras G, Fekete Passa K, Argyropoulou P. Evaluation of five different questionnaires for assessing sleep apnea syndrome in a sleep clinic. Sleep Med. 2014;15(7):776-81. https://doi.org/10.1016/j.sleep.2014.03.012