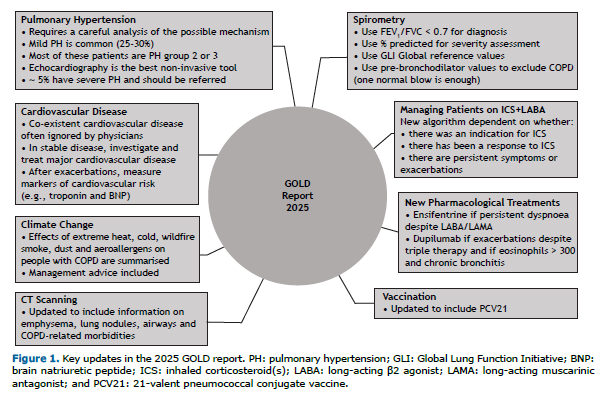
The GOLD reports serve to enable health care professionals to better manage COPD. The GOLD science committee updates the report every year by incorporating the latest evidence relevant to clinical practice, aiming to be as practical and easy to follow as possible. The 2025 GOLD report contains important changes (Figure 1), notably regarding diagnosis and pharmacological management, as well as a new section on climate change and COPD.(1)
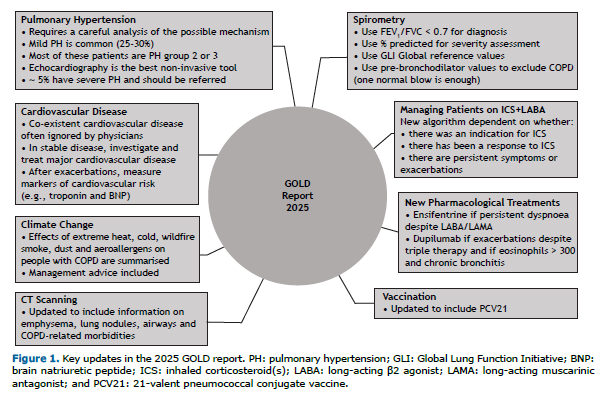
The diagnosis of COPD requires initial clinical assessment of respiratory symptoms and exposure to risk factors. Diagnostic confirmation is obtained using spirometry to demonstrate the presence of airflow obstruction, which is defined as an FEV1/FVC ratio of < 0.7. The 2025 GOLD report considers the merits of using pre- or post-bronchodilator measurements for this purpose. Large cohort studies have demonstrated that although pre-bronchodilator spirometry and post-bronchodilator spirometry give the same diagnostic results in the majority of individuals, post-bronchodilator values can result in up to 36% fewer diagnoses due to a “flow” response characterised by an increase in FEV1 that pushes FEV1/FVC > 0.7.(2) However, administration of a bronchodilator can reduce gas trapping (“volume” response). This improves FVC, thereby reducing the FEV1/FVC ratio; there are a small number of “volume” responders who move from > 0.7 to < 0.7 after bronchodilator administration.(2) The 2025 GOLD report recommends using pre-bronchodilator spirometry > 0.7 to rule out COPD, unless a volume responder is suspected on the basis of low FEV1 or a high symptom burden. This recommendation can avoid unnecessary post-bronchodilator spirometry being performed. If pre-bronchodilator spirometry is < 0.7, then post-bronchodilator measurements are needed for diagnostic confirmation. Flow responders who move to > 0.7 after bronchodilator administration have a high prevalence of developing COPD over time and need careful prospective monitoring.(3) There has been considerable debate concerning the use of the fixed ratio (0.7) versus lower limit of normal (LLN) values (which classify the bottom 5% of the healthy population as abnormal) for diagnostic purposes. The 2025 GOLD report includes some discussion on this issue. The LLN depends on the reference equation used, which are mostly based on pre-bronchodilator values that will over-estimate the number of cases.(2,4) On the basis of simplicity for a worldwide diagnostic test and the fact that there is no absolute right or wrong, GOLD continues to recommend the use of the fixed ratio over the LLN.
Clinical trials in COPD patients with a history of exacerbations in the previous year have consistently demonstrated superiority of triple therapy over the combination of an inhaled corticosteroid (ICS) and a long-acting β2 agonist (LABA) for exacerbation prevention, lung function and quality of life.(5,6) Exacerbations have important detrimental effects on other outcomes, including prolonged impaired quality of life, greater lung function loss and increased mortality. Given the clinical importance of exacerbation prevention, GOLD recommends triple therapy over the ICS-LABA combination if treatment with ICS is indicated. For patients who have been historically treated with the ICS-LABA combination, there is an opportunity to optimise treatment. The 2025 GOLD report includes a new algorithm to help decide the next step, which may include escalation to triple therapy for patients who currently have exacerbations and have blood eosinophil counts > 100 cells/µL (a marker of corticosteroid-sensitive inflammation). For patients who are not currently exacerbating, it is crucial to understand whether there was no prior history of exacerbations, and therefore inappropriate use of ICS, or if previous exacerbations responded to ICS treatment, because this changes the next step.
The 2025 GOLD report includes recommendations on two novel classes of medications to treat COPD: a dual phosphodiesterase 3 (PDE3)/phosphodiesterase 4 (PDE4) inhibitor and the first biologic therapy to be approved for COPD. The inhaled PDE3/PDE4 inhibitor ensifentrine has both anti-inflammatory activity and bronchodilator effects. It significantly improved lung function and dyspnoea but had inconsistent effects on quality of life in parallel phase III studies(7); however, the studies did not assess the impact of ensifentrine on top of LABA plus a long-acting muscarinic antagonist (LAMA) or LABA+LAMA+ICS, making it difficult to assess the relevance of its effects on exacerbations when positioning it in the treatment algorithm. The 2025 GOLD report recommends that ensifentrine be added to dual bronchodilator therapy if the patient continues to experience dyspnoea.
Dupilumab is a fully human monoclonal antibody that blocks the shared IL4 and IL13 receptor. It reduced exacerbation rate and improved lung function and health status in two large randomised trials.(8,9) The patients in those studies all had chronic bronchitis; a history of two or more moderate exacerbations or one or more severe exacerbations in the last year despite treatment with LABA+LAMA+ICS; and blood eosinophil counts ≥ 300 cells/µL. Reflecting the trial entry criteria, the 2025 GOLD report recommends that dupilumab be added to triple therapy if patients continue to have exacerbations and have a blood eosinophil count ≥ 300 cells/µL and symptoms of chronic bronchitis.
It is well known that the prevalence of cardiovascular disease is high in COPD patients. Cardiovascular disease often goes unnoticed and untreated in patients with COPD.(10) Clinicians are perhaps less aware that the risk of cardiovascular events, including myocardial infarction and stroke, increases during and after an exacerbation.(10,11) Although the mechanisms remain to be fully elucidated, systemic inflammation and hypoxia are likely to play key roles in causing cardiovascular stress. A post-hoc analysis has recently demonstrated that triple therapy reduces cardiovascular events in comparison with LAMA/LABA, presumably through exacerbation prevention.(12) The 2025 GOLD report includes a new section on cardiovascular risk, with the aim of raising awareness and encouraging proactive investigation and therapeutic intervention. It also includes a more detailed section on pulmonary hypertension and its investigation and management in patients with COPD, as well as updated sections on vaccination and the role of CT scanning in assessing emphysema, lung nodules, airways and COPD-related comorbidities.
The 2025 GOLD report includes a new section on climate change and the impact of the more frequent and extreme weather events it has caused on people with COPD. Extreme heat and cold are both associated with an increased risk of death in people with COPD,(13-15) with the risk being greater with cold.(16,17) High outdoor temperatures are also associated with an increased risk of hospitalisation for COPD,(15,18,19) as well as with increased dyspnoea and use of short-acting β2 agonists,(20,21) whilst lower outdoor temperatures are associated with an increased risk of exacerbations, increased cough and sputum, increased use of short-acting β2 agonists and a fall in FEV1.(20,22-25) Weather also has a significant impact on air quality, and several studies have examined the interactive effects of pollution and temperature in people with COPD. There appears to be a greater effect of pollutants on COPD hospital admissions and emergency visits at low temperatures or during winter.(26-28)
GOLD recommends that patients keep adequately hydrated, keep out of the heat and try to keep living spaces at temperatures of < 32°C and sleeping spaces at temperatures of < 24°C during heatwaves, as well as keeping bedroom temperatures above 18°C during cold weather, as recommended by the WHO. Prior identification and management of cardiovascular comorbidities are also important to reduce adverse outcomes. The 2025 GOLD report also points out that the selection of inhalers and the correct disposal of inhalers by patients can have important implications for global warming and climate changes, and these should be considered when prescribing therapy.
The GOLD reports provide recommendations on the diagnosis and assessment of patients with COPD, as well as comprehensive recommendations on the management of stable disease, exacerbations and comorbidities. The updates and additions in the 2025 report ensure that these reflect the current evidence base and include newly available treatment options.
REFERENCES 1. Global Initiative for Chronic Obstructive Lung Disease [homepage on the Internet]. Bethesda: GOLD; Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2025 Report. Available from: http://www.goldcopd.org
2. Singh D, Stockley R, Anzueto A, Agusti A, Bourbeau J, Celli BR, et al. GOLD Science Committee recommendations for the use of pre- and post-bronchodilator spirometry for the diagnosis of COPD. Eur Respir J. 2024. Published online January 30, 2025. https://doi.org/10.1183/13993003.01603-2024
3. Fortis S, Eberlein M, Georgopoulos D, Comellas AP. Predictive value of prebronchodilator and postbronchodilator spirometry for COPD features and outcomes. BMJ Open Respir Res. 2017;4(1):e000213. https://doi.org/10.1136/bmjresp-2017-000213
4. Malinovschi A, Zhou X, Andersson A, Backman H, Bake B, Blomberg A, et al. Consequences of Using Post- or Pre-Bronchodilator Reference Values in Interpreting Spirometry. Am J Respir Crit Care Med. 2023;208(4):461-471. https://doi.org/10.1164/rccm.202212-2341OC
5. Lipson DA, Barnhart F, Brealey N, Brooks J, Criner GJ, Day NC, et al. Once-Daily Single-Inhaler Triple versus Dual Therapy in Patients with COPD. N Engl J Med. 2018;378(18):1671-80. https://doi.org/10.1056/NEJMoa1713901
6. Rabe KF, Martinez FJ, Ferguson GT, Wang C, Singh D, Wedzicha JA, et al. Triple Inhaled Therapy at Two Glucocorticoid Doses in Moderate-to-Very-Severe COPD. N Engl J Med. 2020;383(1):35-48. https://doi.org/10.1056/NEJMoa1916046
7. Anzueto A, Barjaktarevic IZ, Siler TM, Rheault T, Bengtsson T, Rickard K, et al. Ensifentrine, a Novel Phosphodiesterase 3 and 4 Inhibitor for the Treatment of Chronic Obstructive Pulmonary Disease: Randomized, Double-Blind, Placebo-controlled, Multicenter Phase III Trials (the ENHANCE Trials). Am J Respir Crit Care Med. 2023;208(4):406-16. https://doi.org/10.1164/rccm.202306-0944OC
8. Bhatt SP, Rabe KF, Hanania NA, Vogelmeier CF, Cole J, Bafadhel M, et al. Dupilumab for COPD with Type 2 Inflammation Indicated by Eosinophil Counts. N Engl J Med. 2023;389(3):205-14. https://doi.org/10.1056/NEJMoa2303951
9. Bhatt SP, Rabe KF, Hanania NA, Vogelmeier CF, Bafadhel M, Christenson SA, et al. Dupilumab for COPD with Blood Eosinophil Evidence of Type 2 Inflammation. N Engl J Med. 2024;390(24):2274-83. https://doi.org/10.1056/NEJMoa2401304
10. Singh D, Han MK, Hawkins NM, Hurst JR, Kocks JWH, Skolnik N, et al. Implications of Cardiopulmonary Risk for the Management of COPD: A Narrative Review. Adv Ther. 2024;41(6):2151-67. https://doi.org/10.1007/s12325-024-02855-4
11. Halpin DM, Decramer M, Celli B, Kesten S, Leimer I, Tashkin DP. Risk of nonlower respiratory serious adverse events following COPD exacerbations in the 4-year UPLIFT(R) trial. Lung. 2011;189(4):261-8. https://doi.org/10.1007/s00408-011-9301-8
12. Singh D, Martinez FJ, Hurst JR, Han MK, Gale CP, Fredriksson M, et al. Effect of Triple Therapy on Cardiovascular and Severe Cardiopulmonary Events in COPD: A Post-hoc Analysis of a Randomized, Double-Blind, Phase 3 Clinical Trial (ETHOS). Am J Respir Crit Care Med. 2024. Epub 2024/08/30. https://doi.org/10.1164/rccm.202312-2311OC
13. Schwartz J. Who is sensitive to extremes of temperature?: A case-only analysis. Epidemiology. 2005;16(1):67-72. https://doi.org/10.1097/01.ede.0000147114.25957.71
14. Davie GS, Baker MG, Hales S, Carlin JB. Trends and determinants of excess winter mortality in New Zealand: 1980 to 2000. BMC Public Health. 2007;7:263. Epub 2007/09/26. https://doi.org/10.1186/1471-2458-7-263
15. Hansel NN, McCormack MC, Kim V. The Effects of Air Pollution and Temperature on COPD. COPD. 2016;13(3):372-9. https://doi.org/10.3109/15412555.2015.1089846
16. Burkart KG, Brauer M, Aravkin AY, Godwin WW, Hay SI, He J, et al. Estimating the cause-specific relative risks of non-optimal temperature on daily mortality: a two-part modelling approach applied to the Global Burden of Disease Study. Lancet. 2021;398(10301):685-97. https://doi.org/10.1016/S0140-6736(21)01700-1
17. Bai J, Cui J, Yu C. Burden of chronic obstructive pulmonary disease attributable to non-optimal temperature from 1990 to 2019: a systematic analysis from the Global Burden of Disease Study 2019. Environ Sci Pollut Res Int. 2023;30(26):68836-47. https://doi.org/10.1007/s11356-023-27325-2
18. Lin S, Luo M, Walker RJ, Liu X, Hwang SA, Chinery R. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology. 2009;20(5):738-46. https://doi.org/10.1097/EDE.0b013e3181ad5522
19. Anderson GB, Dominici F, Wang Y, McCormack MC, Bell ML, Peng RD. Heat-related emergency hospitalizations for respiratory diseases in the Medicare population. Am J Respir Crit Care Med. 2013;187(10):1098-103. https://doi.org/10.1164/rccm.201211-1969OC
20. Scheerens C, Nurhussien L, Aglan A, Synn AJ, Coull BA, Koutrakis P, et al. The impact of personal and outdoor temperature exposure during cold and warm seasons on lung function and respiratory symptoms in COPD. ERJ Open Res. 2022;8(1):00574-2021. https://doi.org/10.1183/23120541.00574-2021
21. McCormack MC, Belli AJ, Waugh D, Matsui EC, Peng RD, Williams DL, et al. Respiratory Effects of Indoor Heat and the Interaction with Air Pollution in Chronic Obstructive Pulmonary Disease. Ann Am Thorac Soc. 2016;13(12):2125-31. https://doi.org/10.1513/AnnalsATS.201605-329OC
22. Tseng CM, Chen YT, Ou SM, Hsiao YH, Li SY, Wang SJ, et al. The effect of cold temperature on increased exacerbation of chronic obstructive pulmonary disease: a nationwide study. PLoS ONE. 2013;8(3):e57066. https://doi.org/10.1371/journal.pone.0057066
23. Mu Z, Chen PL, Geng FH, Ren L, Gu WC, Ma JY, et al. Synergistic effects of temperature and humidity on the symptoms of COPD patients. Int J Biometeorol. 2017;61(11):1919-1925. https://doi.org/10.1007/s00484-017-1379-0
24. Donaldson GC, Seemungal T, Jeffries DJ, Wedzicha JA. Effect of temperature on lung function and symptoms in chronic obstructive pulmonary disease. Eur Respir J. 1999;13(4):844-9. https://doi.org/10.1034/j.1399-3003.1999.13d25.x
25. McCormack MC, Paulin LM, Gummerson CE, Peng RD, Diette GB, Hansel NN. Colder temperature is associated with increased COPD morbidity. Eur Respir J. 2017;49(6):1601501. https://doi.org/10.1183/13993003.01501-2016
26. Qiu H, Tan K, Long F, Wang L, Yu H, Deng R, et al. The Burden of COPD Morbidity Attributable to the Interaction between Ambient Air Pollution and Temperature in Chengdu, China. Int J Environ Res Public Health. 2018;15(3):492. https://doi.org/10.3390/ijerph15030492
27. Ko FW, Tam W, Wong TW, Chan DP, Tung AH, Lai CK, et al. Temporal relationship between air pollutants and hospital admissions for chronic obstructive pulmonary disease in Hong Kong. Thorax. 2007;62(9):780-5. https://doi.org/10.1136/thx.2006.076166
28. Ren C, Williams GM, Tong S. Does particulate matter modify the association between temperature and cardiorespiratory diseases? Environ Health Pers-pect. 2006;114(11):1690-6. https://doi.org/10.1289/ehp.9266


 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Pocket
Pocket