ABSTRACT
Objective: To determine the characteristics of individuals with asthma who are responsive to aerobic training. Methods: This post hoc analysis of pooled data from previous randomized controlled trials involved 101 individuals with moderate to severe asthma who underwent aerobic training. Participants underwent a maximal cardiopulmonary exercise test and completed the Asthma Control Questionnaire and the Asthma Quality of Life Questionnaire before and after a 24-session aerobic training program. Better and worse responders to aerobic training were identified by cluster analysis. Results: Two clusters were identified according to the improvement in peak VO2 after aerobic training (better and worse responders). Characteristics of the better responder group were being older, being female, having higher BMI, and having higher cardiac reserve at baseline when compared with the worse responder group. Also, better responders had worse clinical control, worse quality of life, and lower physical capacity at baseline. After training, worse responders, in comparison with better responders, showed half the improvement in ?peak VO2 (7.4% vs. 13.6%; 95% CI, -12.1 to -0.92%; p < 0.05) and worse asthma control. A weak, negative, but significant association (r = -0.35; p < 0.05) was observed between clinical control and aerobic fitness only in the better responder group. Both groups showed significant improvement in quality of life. Conclusions: Obese individuals with worse exercise capacity, clinical control, and quality of life showed improvement with aerobic training. Moreover, worse responders also improved with training, but to a lesser extent.
Keywords:
Asthma; Exercise therapy; Cluster analysis; Status Asthmaticus; Quality of Life; Rehabilitation.
RESUMO
Objetivo: Determinar as características de indivíduos com asma responsivos a treinamento aeróbio. Métodos: Esta análise post hoc de dados agrupados provenientes de ensaios clínicos controlados randomizados anteriores envolveu 101 indivíduos com asma moderada a grave submetidos a treinamento aeróbico. Os participantes foram submetidos a um teste de exercício cardiopulmonar máximo e responderam ao Asthma Control Questionnaire e ao Asthma Quality of Life Questionnaire antes e depois de um programa de treinamento aeróbio de 24 sessões. Melhores e piores respondedores ao treinamento aeróbio foram identificados por análise de conglomerados. Resultados: Foram identificados dois conglomerados de acordo com a melhora do VO2 de pico após o treinamento aeróbio (melhores e piores respondedores). As características do grupo melhor respondedor foram maior idade, sexo feminino, IMC mais elevado e maior reserva cardíaca basal em comparação com o grupo pior respondedor. Os melhores respondedores também apresentavam pior controle clínico, pior qualidade de vida e menor capacidade física basal. Após o treinamento, os piores respondedores, em comparação com os melhores respondedores, apresentaram metade da melhora no ΔVO2 de pico (7,4% vs. 13,6%; IC95%: -12,1 a -0,92%; p < 0,05) e pior controle da asma. Observou-se uma associação negativa fraca, mas significativa (r = −0,35; p < 0,05) entre controle clínico e aptidão aeróbia apenas no grupo melhor respondedor. Ambos os grupos apresentaram melhora significativa da qualidade de vida. Conclusões: Os indivíduos obesos com pior capacidade de exercício, controle clínico e qualidade de vida apresentaram melhora com o treinamento aeróbio. Além disso, os piores respondedores também melhoraram com o treinamento, mas em menor grau.
Palavras-chave:
Asma; Terapia por exercício; Análise por conglomerados; Estado asmático; Qualidade de vida; Reabilitação.
INTRODUÇÃO A asma é definida como uma doença heterogênea, geralmente caracterizada por inflamação crônica das vias aéreas.(1) A asma leva a inflamação sistêmica, broncoespasmo induzido pelo exercício e desenvolvimento de comorbidades. Além disso, essa condição promove aumento dos níveis de ansiedade e depressão e redução dos níveis de atividade física, levando à redução da capacidade física desses indivíduos.(2) No entanto, o aumento da capacidade de exercício por meio de treinamento físico de intensidade moderada em indivíduos com asma melhora as respostas imunes e reduz a inflamação das vias aéreas.(3) O exercício também diminui a broncoconstrição induzida pelo exercício(3) e o uso de corticosteroides.(4) Além disso, o treinamento físico em indivíduos com asma moderada a grave melhora o controle clínico da asma(5,6) e os fatores de saúde relacionados à qualidade de vida do indivíduo(3,7); por outro lado, a associação entre aptidão física e controle clínico ainda é pouco compreendida.
Ainda não se sabe quem se beneficiaria mais de um programa de treinamento físico(8) e se haveria um determinado subgrupo de indivíduos que não respondem a um programa de treinamento específico.(9) A reabilitação pulmonar é um programa caro e demorado. Ambrosino e Clini(10) afirmaram a importância de se conhecer os preditores de um programa de reabilitação pulmonar de sucesso em indivíduos com DPOC para otimizar o uso de recursos financeiros nessa área. A resposta a um programa de reabilitação pulmonar é multidimensional. (11) Por exemplo, pacientes com DPOC respondedores à reabilitação pulmonar apresentavam sintomas de dispneia mais graves, maior número de hospitalizações, sintomas de ansiedade e depressão mais graves, maior IMC, pior condição de saúde e pior desempenho no exercício antes da intervenção.(11) Outro estudo demonstrou que indivíduos obesos com DPOC que apresentavam melhor função pulmonar e piores níveis de atividade física basal se beneficiaram mais de um programa de reabilitação pulmonar.(12)
Apesar dos benefícios bem conhecidos de melhora da capacidade de exercício em indivíduos com asma, os fatores que determinam aqueles que respondem a um programa de reabilitação pulmonar foram relatados exclusivamente em indivíduos com DPOC. Embora esses fatores possam ser óbvios e possam ser aplicados a outras doenças pulmonares crônicas, a determinação desses fatores é obrigatória em virtude das características específicas e do impacto na vida dos pacientes com asma. Até o momento, não há informações sobre quais indivíduos com asma respondem a treinamento aeróbio ou programas de reabilitação pulmonar. Portanto, este estudo teve como objetivo determinar as características de indivíduos com asma moderada a grave que respondem a treinamento aeróbio e a relação dessa resposta com alterações no controle clínico, na qualidade de vida e na capacidade de exercício.
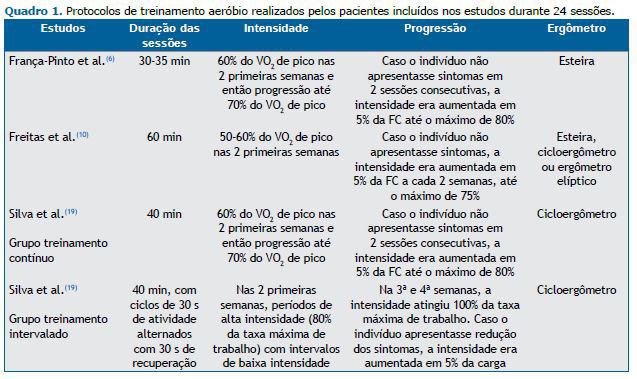
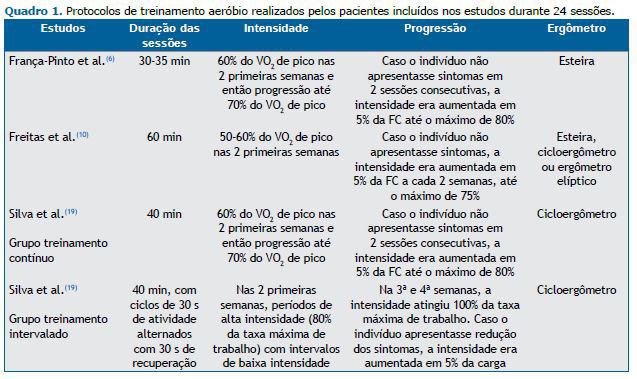
MÉTODOS Trata-se de uma análise post hoc de dados agrupados provenientes de ensaios clínicos controlados randomizados anteriores.(3,6,13) Esses ensaios envolveram indivíduos com asma moderada a grave que haviam participado anteriormente de um programa de reabilitação pulmonar em nosso centro e foram submetidos a treinamento aeróbio (Quadro 1). (3,6,13) Não houve sobreposição de indivíduos entre os estudos. Todos os indivíduos foram acompanhados no mesmo hospital universitário. O comitê de ética em pesquisa da instituição aprovou os estudos clínicos (CAAE n. 0121/10, n. 07137512.9.0000.0068 e n. 18178013.9.0000.0068).(3,6,13) Todos os participantes concluíram o programa de treinamento aeróbio entre 2015 e 2019. As variáveis do teste de exercício cardiopulmonar (TECP), o controle clínico da asma e a qualidade de vida foram avaliados antes e após a intervenção.
Os indivíduos com idade de 20 a 60 anos e diagnóstico de asma (nível de gravidade segundo os critérios estabelecidos pela Global Initiative for Asthma)(1) em cada um dos estudos, com base no nível de tratamento necessário para controlar as exacerbações e sintomas, foram incluídos no presente estudo. Os indivíduos deveriam ter tido acompanhamento médico por pelo menos seis meses, utilizando tratamento médico otimizado para asma, e apresentado estabilidade clínica (pelo menos 30 dias sem necessidade de troca de medicamentos, sem visitas ao pronto-socorro e sem hospitalizações).
Os critérios de exclusão foram apresentar outra doença pulmonar crônica, câncer, doença cardiovascular ou disfunções musculoesqueléticas que pudessem interferir nas avaliações e/ou nos exercícios físicos. Além disso, foram excluídas as gestantes, os fumantes e ex-fumantes (≥ 10 anos-maço), aqueles com incapacidade de compreender as instruções dadas pelos pesquisadores e os participantes de outros protocolos de pesquisa.
Todos os indivíduos foram submetidos a um programa de treinamento aeróbio de 24 sessões. Os parâmetros de treinamento foram determinados pela avaliação do VO2 durante um TECP pré-reabilitação e foram semelhantes entre os estudos (Quadro 1). Antes e após a intervenção, a função pulmonar foi avaliada por meio de espirometria,(14) e o VEF1 e a CVF foram analisados utilizando os valores previstos para a população brasileira.(15) O controle clínico foi avaliado utilizando a versão brasileira do Asthma Control Questionnaire com 7 itens (ACQ-7).(16) As questões do ACQ-7 estão relacionadas a sintomas, limitações das atividades, dispneia, sibilância e uso de broncodilatador de resgate na última semana.(16) O último item do ACQ- 7 refere-se a uma questão que avalia o VEF1 (em % do valor previsto, pré-broncodilatador). Esse questionário contém sete itens em uma escala de 7 pontos (0 = sem limitação e 6 = limitação máxima). Pontuações mais altas indicam pior controle clínico. Uma pontuação igual ou superior a 1,5 é considerada asma não controlada.(17) Uma mudança de 0,5 ponto na pontuação do ACQ-7 é considerada clinicamente eficaz.(18) Além disso, a qualidade de vida relacionada à saúde na asma foi avaliada por meio da versão brasileira do Asthma Quality of Life Questionnaire (AQLQ).(19) O AQLQ contém 32 itens e é dividido em quatro domínios: limitações das atividades, sintomas, função emocional e exposição ambiental. Pontuações mais altas indicam melhor qualidade de vida. Uma mudança de 0,5 ponto na pontuação do AQLQ é considerada clinicamente eficaz.(20)
A capacidade de exercício foi avaliada por meio de um TECP máximo até o limite da tolerância, realizado em esteira(3) ou cicloergômetro.(6,13) Os protocolos utilizados foram anteriormente estabelecidos para esteira(21,22) e cicloergômetro.(23) A comparação entre os valores de VO2máx previsto obtidos em dois ergômetros foi corrigida de acordo com a equação(24):
VO2máx = 45,2 – 0,35 × idade – 10,9 × sexo – 0,15 × peso + 0,68 × altura – 0,46 × modo de exercício
onde VO2máx é dado em mL·kg–1·min–1; idade, em anos; sexo, como masculino = 1 e feminino = 2; peso, em libras; altura, em polegadas; e modo de exercício, como esteira = 1 e cicloergômetro = 2. Isso foi necessário em virtude da diferença entre o gasto energético avaliado nos dois ergômetros.(25) As variáveis do TECP foram VO2 basal, em mL/min; limiar anaeróbio (LA), em mL·kg–1·min–1; e pico do exercício, em % do previsto.(24) Além disso, Ve, FC máxima e razão de troca respiratória (RER, do inglês respiratory exchange ratio) foram registrados ao final do teste.
Os dados foram analisados quanto à normalidade utilizando o teste de Kolmogorov-Smirnov. A análise de conglomerados foi realizada em duas etapas.(26) Inicialmente, uma análise hierárquica utilizando o método de Ward determinou automaticamente o número de conglomerados. Em seguida, foi realizada a análise do algoritmo k-means para agrupar os indivíduos em conglomerados. A análise de conglomerados foi realizada incluindo as seguintes variáveis: idade; VEF1 (% do previsto); IMC; LA de VO2 (VO2LA) pré-intervenção; VO2 de pico pré-intervenção; Δpontuação do AQLQ (pós/pré-intervenção); Δpontuação do ACQ-7 (pós/pré-intervenção); e ΔVO2 de pico pós/pré-teste. O teste t foi utilizado para comparar os conglomerados. O teste z foi utilizado para comparar proporções entre os conglomerados. Testes de Pearson foram utilizados para analisar a correlação entre ΔVO2 e ΔACQ-7 em ambos os grupos. Foram utilizados o Statistical Package for the Social Sciences, versão 12.0 (SPSS Inc., Chicago, IL, EUA) e o software SigmaStat, versão 3.5 (Systat Software Inc., Chicago, IL, EUA). O nível de significância foi estabelecido em 5% (p < 0,05).
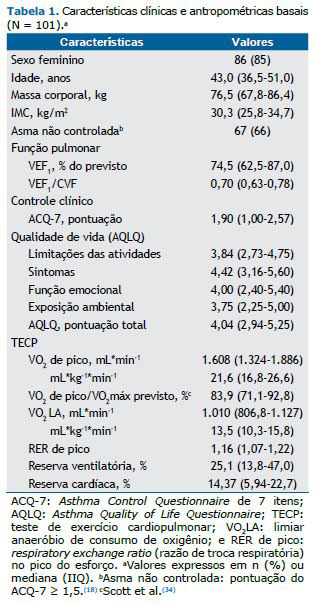
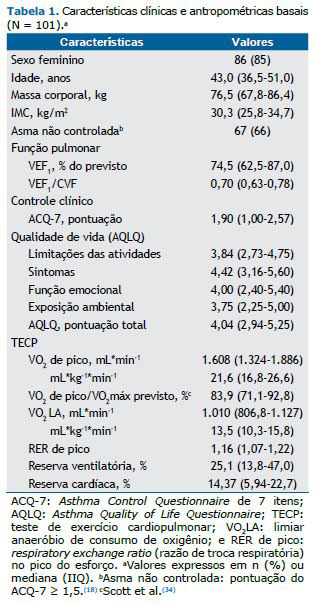
RESULTADOS Este estudo envolveu 101 indivíduos com asma que concluíram um programa de treinamento aeróbio: 22 do estudo de França-Pinto et al.,(3) 26 do estudo de Freitas et al.(6) e 53 do estudo de Aparecido da Silva et al.,(13) alocados em dois grupos: grupo treinamento intervalado e grupo treinamento contínuo.
De todos os indivíduos incluídos, 55 (54,5%) eram obesos (IMC > 30 kg/m2), 49 (48,5%) apresentavam obstrução moderada das vias aéreas (Tabela 1), e 67 (66,3%) tinham asma não controlada. No tocante à resposta ao TECP máximo, 32 (31,7%) dos indivíduos apresentaram limitações no sistema ventilatório, 51 (50,5%), no sistema cardiovascular, e 65 (64,4%), no sistema muscular periférico.
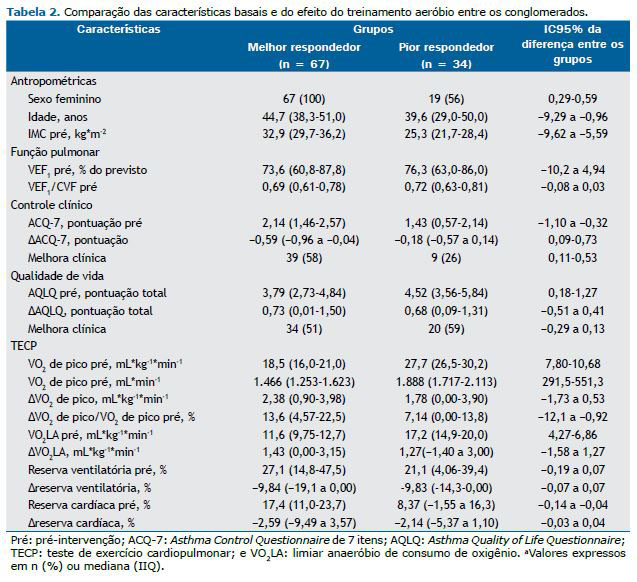
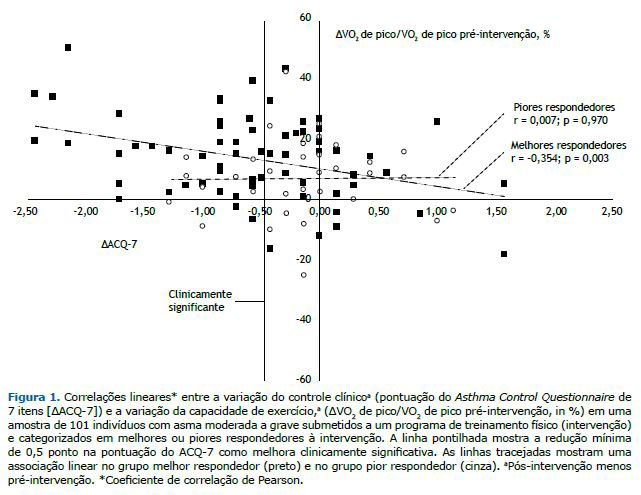
Após a análise de conglomerados, os dois grupos foram determinados com base na melhora do VO2 de pico após o treinamento aeróbio. Os grupos foram classificados em melhores e piores respondedores ao treinamento aeróbio (Tabela 2). Antes da intervenção, o grupo melhor respondedor era composto principalmente por mulheres e indivíduos mais velhos com IMC mais elevado e maior reserva cardíaca em comparação com o grupo pior respondedor. Além disso, o grupo melhor respondedor apresentava pior controle clínico e pior qualidade de vida antes do treinamento e menor capacidade física (VO2 de pico e VO2LA) do que o grupo pior respondedor. Por outro lado, a função pulmonar (VEF1 e relação VEF1/CVF) e a reserva ventilatória eram semelhantes entre os grupos. Após o programa de treinamento, o grupo melhor respondedor apresentou uma melhora duas vezes maior no ΔVO2 de pico do que o grupo pior respondedor. Apenas o grupo melhor respondedor apresentou melhora clinicamente significativa no controle clínico da asma (diminuição ≥ 0,5 na pontuação do ACQ-7), que foi associada à melhora da potência aeróbia (Figura 1)
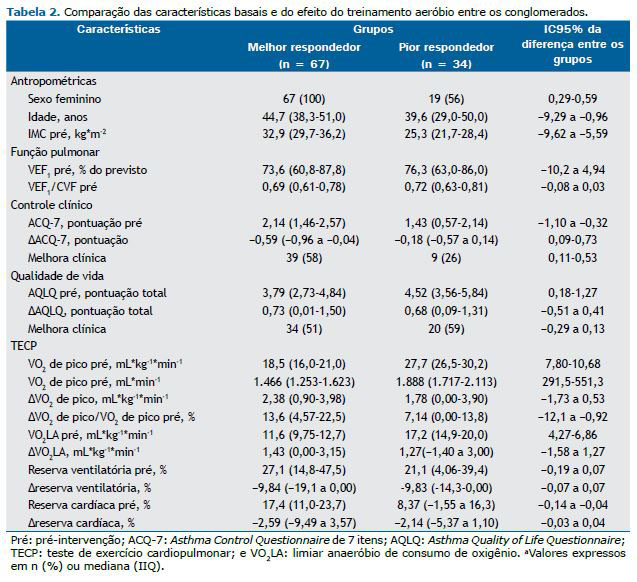
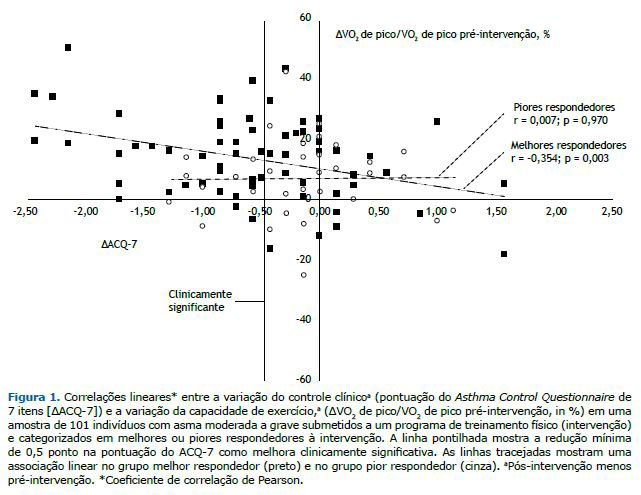
Ambos os grupos apresentaram melhora clinicamente significativa na qualidade de vida relacionada à saúde (aumento ≥ 0,5 na pontuação do AQLQ) após a intervenção (Tabela 2). As reservas cardíaca e respiratória, o VO2LA e o VO2 de pico após o TECP foram semelhantes entre os grupos.
DISCUSSÃO Nossos resultados mostraram as características de indivíduos com asma moderada a grave que responderam significativamente ao treinamento aeróbio. Mulheres e indivíduos mais velhos com IMC mais elevado, bem como com pior capacidade aeróbia, controle clínico e qualidade de vida, apresentaram boa resposta ao treinamento aeróbio. Embora esses resultados pareçam intuitivos, este é o primeiro estudo a investigar tais características clínicas. Além disso, observou-se que ambos os grupos apresentaram melhora clinicamente significativa nos aspectos de saúde relacionados à qualidade de vida.
Várias revisões sistemáticas investigaram os benefícios do exercício físico na melhora da capacidade de exercício, qualidade de vida e sintomas em indivíduos com asma.(27-29) No entanto, há informações limitadas sobre quais indivíduos com asma se beneficiam mais do treinamento aeróbio. Neste estudo, houve predomínio do sexo feminino no grupo melhor respondedor, e duas explicações podem justificar esse achado. Em primeiro lugar, há maior prevalência de mulheres adultas com asma moderada a grave.(30) Em segundo lugar, mulheres de meia-idade tendem a ser mais sedentárias, ter sobrepeso/obesidade e apresentar pior condicionamento físico mesmo quando não têm asma.(31,32) Isso também pode explicar as diferenças de idade entre os grupos. Entretanto, não acreditamos que nossos resultados estabeleçam uma prioridade para treinamento físico em mulheres com asma. Em vez disso, a prioridade deve ser para indivíduos com baixo condicionamento físico, obesidade e doença não controlada clinicamente.
Estudos anteriores relataram que indivíduos não obesos com asma controlada(3,5) e indivíduos obesos com asma não controlada(6) melhoram seu condicionamento aeróbio e sua qualidade de vida após um programa de treinamento físico. Esses achados corroboram nossos resultados, pois não encontramos diferenças na qualidade de vida entre os grupos após o programa de treinamento físico. No entanto, o grupo melhor respondedor apresentou uma melhora duas vezes maior na capacidade aeróbia (ΔVO2 de pico) do que o grupo pior respondedor. Essa melhora não pode ser associada a diferenças entre os programas de treinamento, pois a intensidade do exercício foi estabelecida de forma semelhante com base no TECP em todos os estudos, independentemente da modalidade de treinamento (treinamento contínuo ou intervalado).(13) Da mesma forma, acreditamos que o uso de esteira para metade da amostra em vez de cicloergômetro não interferiu nos resultados, pois todos os participantes melhoraram sua capacidade aeróbia. Nossos resultados indicaram que os indivíduos com asma moderada a grave com LA e potência aeróbia baixos apresentaram maior aumento do condicionamento físico após o treinamento aeróbio.
Indivíduos com asma não controlada antes do treinamento se beneficiam principalmente do controle dos sintomas da asma e apresentam alteração clinicamente significativa (> 0,5 ponto no ACQ-7). (5,6,17) A obesidade e a falta de controle clínico da asma já foram associadas a pior condicionamento físico(30); portanto, é mais comum identificar indivíduos que apresentam mais de um fator associado à resposta ao exercício. Consideramos que a prescrição de treinamento aeróbio para indivíduos com asma deve ser recomendada para aqueles que apresentam falta de controle da asma apesar de tratamento farmacológico otimizado (critérios de inclusão de todos os pacientes do presente estudo). Além disso, nossos resultados confirmam que os benefícios do treinamento físico devem ser analisados de forma diferente em indivíduos com e sem controle da asma em estudos futuros. Essa abordagem pode melhorar nossa compreensão dos efeitos do treinamento físico nessa população.
Três teorias foram sugeridas para explicar como a melhora da capacidade aeróbia em indivíduos com asma reduz os sintomas e melhora o controle da asma: melhora da capacidade ventilatória,(27) melhora da função pulmonar(28) e redução da inflamação pulmonar e sistêmica.(3,6) Nossos resultados mostraram que os indivíduos com asma apresentavam reserva ventilatória basal reduzida (25% em média) em comparação com a população geral (aproximadamente 50%) e próxima ao valor de corte para estabelecer limitação ventilatória (< 20%).(23) Além disso, observamos que os indivíduos com asma apresentavam capacidade aeróbia e reserva cardíaca reduzidas, sugerindo fortemente que eles estavam fisicamente inaptos antes do treinamento físico. Assim, nossos resultados reforçam que o treinamento físico melhora a aptidão aeróbia em indivíduos com asma, exigindo aumento da capacidade ventilatória.
Neste estudo, apenas o grupo melhor respondedor apresentou associação linear entre a melhora do condicionamento físico e o controle clínico. Uma possível explicação para essa associação é que a melhora da aptidão aeróbia melhora a capacidade aeróbia, reduz a ventilação nas atividades cotidianas e reduz os sintomas da asma. Estudos randomizados e controlados anteriores também sugeriram que o treinamento melhora a resposta imune,(3,6) mas uma revisão sistemática sugeriu que não houve efeito na resposta imune dos pacientes com asma.(28) No entanto, a revisão supracitada incluiu pacientes com diferentes níveis de gravidade e controle clínico da asma que podem ter interferido na análise dos dados. Além disso, nem todos os indivíduos incluídos em nosso estudo foram avaliados quanto à inflamação pulmonar e sistêmica, impossibilitando esse tipo de análise.
Antes do treinamento, os indivíduos de ambos os grupos apresentaram menor pontuação do AQLQ em nosso estudo do que em estudos anteriores.(5,7,33,34) Os melhores respondedores ao treinamento aeróbio apresentaram pontuações do AQLQ ainda menores do que os piores respondedores. Após o treinamento, ambos os grupos apresentaram melhora clinicamente significativa, e estudos anteriores corroboram nossos achados.(5,7,33,34) Não houve associação entre a melhora da potência aeróbia e a qualidade de vida. Uma hipótese para esse achado seria o aspecto multifatorial da qualidade de vida. O AQLQ possui vários domínios (limitações das atividades, sintomas, função emocional e exposição ambiental) que podem ser modificados pelo treinamento físico, independentemente do condicionamento físico obtido por cada indivíduo.(20)
Este estudo apresenta limitações. Em primeiro lugar, trata-se de uma análise post hoc de dados agrupados provenientes de ensaios clínicos controlados randomizados anteriores, e não de um estudo prospectivo. No entanto, essa limitação é amenizada pelo número de pacientes e de variáveis avaliadas, e todos os indivíduos foram submetidos a treinamento físico no mesmo centro de pesquisa utilizando uma intensidade de exercício semelhante. Além disso, acreditamos que nenhum outro centro tenha um número tão grande de indivíduos submetidos a treinamento físico, com base em resultados de TECP, sendo avaliados quanto ao controle clínico da asma e a qualidade de vida. Em segundo lugar, a maioria dos indivíduos neste estudo era do sexo feminino; no entanto, isso era esperado em virtude da maior prevalência de asma em indivíduos do sexo feminino e do fato de as mulheres procurarem atendimento médico com mais regularidade do que os homens.(30) Além disso, mulheres com asma apresentam alta prevalência de obesidade e de asma não controlada. No entanto, nossas pacientes do sexo feminino apresentaram uma ampla distribuição de indivíduos obesos e não obesos com asma controlada e não controlada. Em terceiro lugar, o efeito sobre os mediadores inflamatórios não foi incluído, pois apenas dois estudos avaliaram esse desfecho,(6,13) impossibilitando sua inclusão nas análises estatísticas. Além do mais, a força muscular poderia estar associada à resposta do paciente ao programa de treinamento físico, e a melhora da resposta muscular periférica também poderia acrescentar informações importantes; no entanto, essa variável não foi avaliada por nenhum dos estudos aqui incluídos. Por fim, a limitação ao exercício foi categorizada em sistemas cardíaco, ventilatório e muscular periférico, o que pode ser considerado uma forma simplificada de compreender as limitações individuais dos pacientes. No entanto, essa análise já foi considerada em indivíduos com asma(35) e em outras populações.(23) Além disso, não utilizamos essas respostas fisiológicas para determinar o principal motivo pelo qual os pacientes necessariamente interromperiam o teste. Em vez disso, essa análise foi utilizada secundariamente para entender a principal limitação de cada conglomerado.
Os resultados deste estudo mostram que os indivíduos obesos com baixa capacidade de exercício, controle clínico e qualidade de vida obtiveram maiores benefícios do programa de treinamento aeróbio. Portanto, indivíduos com essas características devem ser encaminhados prioritariamente para programas de treinamento aeróbio, a fim de reduzir os sintomas da asma. Os melhores e os piores respondedores ao treinamento aeróbio apresentaram melhoras semelhantes na qualidade de vida.
CONTRIBUIÇÕES DOS AUTORES TCE, ACL, PDF e CRFC: concepção e desenho do estudo. TCE e ACL: análise dos dados e redação do manuscrito. PDF, RAS, FARM e AFP: coleta de dados e revisão crítica do manuscrito. RMCP e CRFC: revisão crítica final do manuscrito. Todos os autores aprovaram o manuscrito final.
CONFLITOS DE INTERESSE Os autores declaram que os resultados do estudo são apresentados de forma clara, honesta e sem fabricação, falsificação ou manipulação inadequada de dados. Os autores declaram não ter conflitos de interesse a revelar.
DECLARAÇÃO DE DISPONIBILIDADE DE DADOS O banco de dados está disponível no repositório: https://zenodo.org/record/6326209#.YyospqTMK5c
REFERÊNCIAS 1. Global Initiative for Asthma (GINA) [homepage on the Internet]. Bethesda: GINA; c2021 [cited 2021 Jul 1]. Global Strategy for Asthma Management and Prevention (Updated 2021). [Adobe Acrobat document, 217p.]. Available from: https://ginasthma.org/wp content/uploads/2021/05/GINA Main Report 2021 V2 WMS.pdf
2. Carvalho Pinto RM, Cançado JED, Pizzichini MMM, Fiterman J, Rubin AS, Cerci Neto A, et al. 2021 Brazilian Thoracic Association recommendations for the management of severe asthma. J Bras Pneumol. 2021;47(6):e20210173. https://doi.org/10.36416/1806-3756/e20210273
3. França-Pinto A, Mendes FA, de Carvalho-Pinto RM, Agondi RC, Cukier A, Stelmach R, et al. Aerobic training decreases bronchial hyperresponsiveness and systemic inflammation in patients with moderate or severe asthma: a randomised controlled trial. Thorax. 2015;70(8):732-739. https://doi.org/10.1136/thoraxjnl-2014-206070
4. Neder JA, Nery LE, Silva AC, Cabral AL, Fernandes AL. Short-term effects of aerobic training in the clinical management of moderate to severe asthma in children. Thorax. 1999;54(3):202-206. https://doi.org/10.1136/thx.54.3.202
5. Dogra S, Kuk JL, Baker J, Jamnik V. Exercise is associated with improved asthma control in adults. Eur Respir J. 2011;37(2):318-323. https://doi.org/10.1183/09031936.00182209
6. Freitas PD, Ferreira PG, Silva AG, Stelmach R, Carvalho-Pinto RM, Fernandes FL, et al. The Role of Exercise in a Weight-Loss Program on Clinical Control in Obese Adults with Asthma. A Randomized Controlled Trial. Am J Respir Crit Care Med. 2017;195(1):32-42. https://doi.org/10.1164/rccm.201603-0446OC
7. Turner S, Eastwood P, Cook A, Jenkins S. Improvements in symptoms and quality of life following exercise training in older adults with moderate/severe persistent asthma. Respiration. 2011;81(4):302-310. https://doi.org/10.1159/000315142
8. Herigstad M, Faull OK, Hayen A, Evans E, Hardinge FM, Wiech K, et al. Treating breathlessness via the brain: changes in brain activity over a course of pulmonary rehabilitation. Eur Respir J. 2017;50(3):1701029. https://doi.org/10.1183/13993003.01029-2017
9. Montero D, Lundby C. Refuting the myth of non-response to exercise training: ‘non-responders’ do respond to higher dose of training [published correction appears in J Physiol. 2018 Apr 1;596(7):1311]. J Physiol. 2017;595(11):3377-3387. https://doi.org/10.1113/JP273480
10. Ambrosino N, Clini EM. Response to pulmonary rehabilitation: toward personalised programmes?. Eur Respir J. 2015;46(6):1538-1540. https://doi.org/10.1183/13993003.01125-2015
11. Spruit MA, Augustin IM, Vanfleteren LE, Janssen DJ, Gaffron S, Pennings HJ, et al. Differential response to pulmonary rehabilitation in COPD: multidimensional profiling. Eur Respir J. 2015;46(6):1625-1635. https://doi.org/10.1183/13993003.00350-2015
12. Buekers J, DE Boever P, Theunis J, Houben-Wilke S, Vaes AW, Franssen FME, et al. Physiological Changes Differ between Responders and Nonresponders to Pulmonary Rehabilitation in COPD. Med Sci Sports Exerc. 2021;53(6):1125-1133. https://doi.org/10.1249/MSS.0000000000002578
13. Aparecido da Silva R, Leite Rocco PG, Stelmach R, Mara da Silva Oliveira L, Sato MN, Cukier A, et al. Constant-Load Exercise Versus High-Intensity Interval Training on Aerobic Fitness in Moderate-to-Severe Asthma: A Randomized Controlled Trial. J Allergy Clin Immunol Pract. 2022;10(10):2596-2604.e7. https://doi.org/10.1016/j.jaip.2022.05.023
14. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al; ATS/ERS Task Force. Standardisation of spirometry. Eur Respir J. 2005;26(2):319-338. https://doi.org/10.1183/09031936.05.00034805
15. Pereira CA, Sato T, Rodrigues SC. New reference values for forced spirometry in white adults in Brazil. J Bras Pneumol. 2007;33(4):397-406. https://doi.org/10.1590/S1806-37132007000400008
16. Leite M, Ponte EV, Petroni J, D’Oliveira Júnior A, Pizzichini E, Cruz AA. Evaluation of the asthma control questionnaire validated for use in Brazil. J Bras Pneumol. 2008;34(10):756-763. https://doi.org/10.1590/S1806-37132008001000002
17. Juniper EF, Bousquet J, Abetz L, Bateman ED; GOAL Committee. Identifying ‘well-controlled’ and ‘not well-controlled’ asthma using the Asthma Control Questionnaire. Respir Med. 2006;100(4):616-621. https://doi.org/10.1016/j.rmed.2005.08.012
18. Juniper EF, Svensson K, Mörk AC, Ståhl E. Measurement properties and interpretation of three shortened versions of the asthma control questionnaire. Respir Med. 2005;99(5):553-558. https://doi.org/10.1016/j.rmed.2004.10.008
19. De Oliveira MA, Barbiere A, Santos LA, Faresin SM, Fernandes AL. Validation of a simplified quality-of-life questionnaire for socioeconomically deprived asthma patients. J Asthma. 2005;42(1):41-44. https://doi.org/10.1081/JAS-200044772
20. Juniper EF, Guyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific Quality of Life Questionnaire. J Clin Epidemiol. 1994;47(1):81-87. https://doi.org/10.1016/0895-4356(94)90036-1
21. Heyward VH. Advanced fitness assessment and exercise prescription. Champaign, IL: Human Kinetics; 1997. p. 322.
22. Santos-Silva PR, Fonseca AJ, Castro AW, Greve JM, Hernandez AJ. Reproducibility of maximum aerobic power (VO2max) among soccer players using a modified heck protocol. Clinics (Sao Paulo). 2007;62(4):391-396. https://doi.org/10.1590/S1807-59322007000400004
23. Wasserman K, Hansen JE, Sue DY, Casaburi R, Whipp BJ. Pathophysiology of disorders limiting exercise. In: Principles of Exercise Testing and Interpretation. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 1999. p. 1142-1195.
24. de Souza E Silva CG, Kaminsky LA, Arena R, Christle JW, Araújo CGS, Lima RM, et al. A reference equation for maximal aerobic power for treadmill and cycle ergometer exercise testing: Analysis from the FRIEND registry. Eur J Prev Cardiol. 2018;25(7):742-750. https://doi.org/10.1177/2047487318763958
25. American Thoracic Society; American College of Chest Physicians. ATS/ACCP Statement on cardiopulmonary exercise testing [published correction appears in Am J Respir Crit Care Med. 2003 May 15;1451-2]. Am J Respir Crit Care Med. 2003;167(2):211-277. https://doi.org/10.1164/rccm.167.2.211
26. Cluster analysis. In: Mooi E, Sarstedt M. A Concise Guide to Market Research. Berlin, Heidelberg: Springer-Verlag; 2011. p. 237-284. https://doi.org/10.1007/978-3-642-12541-6_9
27. Ram FS, Robinson SM, Black PN. Effects of physical training in asthma: a systematic review. Br J Sports Med. 2000;34(3):162-167. https://doi.org/10.1136/bjsm.34.3.162
28. Hansen ESH, Pitzner-Fabricius A, Toennesen LL, Rasmusen HK, Hostrup M, Hellsten Y, et al. Effect of aerobic exercise training on asthma in adults: a systematic review and meta-analysis. Eur Respir J. 2020;56(1):2000146. https://doi.org/10.1183/13993003.00146-2020
29. Kuder MM, Clark M, Cooley C, Prieto-Centurion V, Danley A, Riley I, Siddiqi A, et al. A Systematic Review of the Effect of Physical Activity on Asthma Outcomes. J Allergy Clin Immunol Pract. 2021;9(9):3407-3421.e8. https://doi.org/10.1016/j.jaip.2021.04.048
30. de Carvalho-Pinto RM, Cukier A, Angelini L, Antonangelo L, Mauad T, Dolhnikoff M, et al. Clinical characteristics and possible phenotypes of an adult severe asthma population. Respir Med. 2012;106(1):47-56. https://doi.org/10.1016/j.rmed.2011.08.013
31. Ribeiro MA, Martins MA, Carvalho CR. Interventions to increase physical activity in middle-age women at the workplace: a randomized controlled trial. Med Sci Sports Exerc. 2014;46(5):1008-1015. https://doi.org/10.1249/MSS.0000000000000190
32. Freitas PD, Xavier RF, McDonald VM, Gibson PG, Cordova-Rivera L, Furlanetto KC, et al. Identification of asthma phenotypes based on extrapulmonary treatable traits. Eur Respir J. 2021;57(1):2000240. https://doi.org/10.1183/13993003.00240-2020
33. Pakhale S, Baron J, Dent R, Vandemheen K, Aaron SD. Effects of weight loss on airway responsiveness in obese adults with asthma: does weight loss lead to reversibility of asthma?. Chest. 2015;147(6):1582-1590. https://doi.org/10.1378/chest.14-3105
34. Scott HA, Gibson PG, Garg ML, Pretto JJ, Morgan PJ, Callister R, et al. Dietary restriction and exercise improve airway inflammation and clinical outcomes in overweight and obese asthma: a randomized trial. Clin Exp Allergy. 2013;43(1):36-49. https://doi.org/10.1111/cea.12004
35. Ferreira PG, Freitas PD, Silva AG, Porras DC, Stelmach R, Cukier A, et al. Dynamic hyperinflation and exercise limitations in obese asthmatic women. J Appl Physiol (1985). 2017;123(3):585-593. https://doi.org/10.1152/japplphysiol.00655.2016