BACKGROUND Dyspnea and exercise intolerance are hallmarks of pulmonary hypertension (PH). Extant knowledge in the field has mostly accrued from studies involving patients with pulmonary arterial hypertension.(1) Less is known on the determinants of exertional dyspnea in chronic thromboembolic PH,(2) a much more frequent cause of PH in clinical practice.
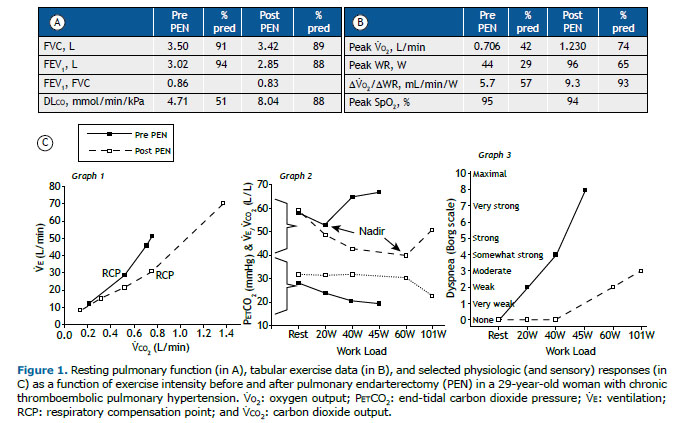
OVERVIEW A non-smoking 29-year-old woman complained of progressive dyspnea — modified Medical Research Council (mMRC) scale score = 4 — after pulmonary thromboembolism with a high clot burden two years earlier. Unremarkable spirometry coexisted with a moderate reduction in DLCO (Figure 1A). Echocardiography unveiled PH, and right heart catheterization confirmed precapillary PH. After a pulmonary CT angiogram demonstrating residual filling defects in the pulmonary arteries to the lower lobes, the patient underwent pulmonary endarterectomy (PEN). Improvement in dyspnea during activities of daily living (mMRC = 1) after surgery was accompanied by a significant increase in DLCO (Figure 1A) and O2 uptake (V̇O2) at a given work rate (WR) and at peak exercise (Figure 1B). A decrease in ventilation (V̇E) requirements for a given CO2 output (V̇CO2) from the start of exercise, together with a delayed respiratory compensation point (RCP) to lactic acidosis were associated with lower dyspnea scores throughout exercise (Figure 1C).
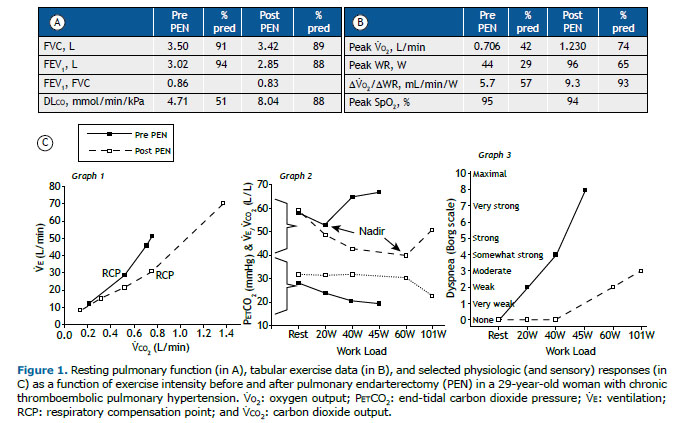
In healthy subjects, pulmonary gas exchange efficiency improves during exercise since a lower fraction of VT is wasted in the physiological (anatomical plus alveolar) dead space (VDphys). Thus, less V̇E is needed to clear a given amount of CO2, that is, V̇E/V̇CO2 decreases down to a low minimum (nadir; Figure 1C, Graph 2). If VDphys does not improve as expected (or even increases) (a) and/or the subject hyperventilates dropping PaCO2 (b), V̇E/V̇CO2 increases, bringing shortness of breath.(3) The relative importance of (a) or (b) to increase V̇E/V̇CO2 seems to vary, depending on the location of the occluding clots: whereas proximal, larger-vessel disease markedly increases VDphys since blood flow is reduced over a large portion of the vascular tree (a), increased neurochemical stimulation leading to hyperventilation (b) has a greater contributory role in distal, smaller-vessel disease.(4) End-tidal PCO2 is characteristically reduced in chronic thromboembolic PH (Figure 1C, Graph 2, bottom) secondary to impaired perfusion of ventilated alveoli decreasing the rate of CO2 “unloading” from mixed venous blood to alveoli (a) and/or due to alveolar hyperventilation (b).(5) In the current patient, PEN led to a dramatic decrease in the ventilatory requirements during exercise (Figure 1C, Graphs 1 and 2) and enhanced central hemodynamics, leading to higher O2 delivery to the contracting muscles (higher V̇O2/WR), which delayed the onset of metabolic acidosis (RCP). These factors, together with lower pulmonary vascular pressures, likely contributed to decreased neural drive to breathe. Jointly, these mechanisms explain why the patient required 25 L/min less V̇E to clear 1 L/min V̇CO2 at 45 W (V̇E/V̇CO2 declined from 67 L/L to 42 L/L); consequently, dyspnea intensity decreased from “very intense” to ”light” (Figure 1C, Graph 3).
CLINICAL MESSAGE Lessening the ventilatory requirements for exercise has major beneficial effects on dyspnea in patients with PH. Therapeutic approaches that improve pulmonary gas exchange efficiency and cardiocirculatory function (peripheral O2 delivery) are poised to reduce breathing discomfort, enhancing exercise tolerance of patients.
REFERENCES 1. Neder JA, Ramos RP, Ota-Arakaki JS, Hirai DM, D’Arsigny CL, O’Donnell D. Exercise intolerance in pulmonary arterial hypertension. The role of cardiopulmonary exercise testing. Ann Am Thorac Soc. 2015;12(4):604-612. https://doi.org/10.1513/AnnalsATS.201412-558CC
2. Ramos RP, Ferreira EVM, Valois FM, Cepeda A, Messina CMS, Oliveira RK, Araújo ATV, et al. Clinical usefulness of end-tidal CO2 profiles during incremental exercise in patients with chronic thromboembolic pulmonary hypertension. Respir Med. 2016;120:70-77. https://doi.org/10.1016/j.rmed.2016.09.020
3. Neder JA, Berton DC, O’Donnell DE. Out-of-proportion dyspnea and exercise intolerance in mild COPD. J Bras Pneumol. 2021;47(3):e20210205. https://doi.org/10.36416/1806-3756/e20210205
4. Zhai Z, Murphy K, Tighe H, Wang C, Wilkins MR, Gibbs JSR, et al. Differences in ventilatory inefficiency between pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension. Chest. 2011;140(5):1284-1291. https://doi.org/10.1378/chest.10-3357
5. Neder JA. Residual Exertional Dyspnea in Cardiopulmonary Disease. Ann Am Thorac Soc. 2020;17(12):1516-1525. https://doi.org/10.1513/AnnalsATS.202004-398FR