ABSTRACT
Objective: The objective of this study is to evaluate the impact of social distancing resulting from COVID-19 in hospitalizations for infections of the upper airways (URTI), such as acute laryngitis, tracheitis, and otitis media in children aged 0 to 9 years in Brazil, considering that they share the same forms of transmission. Methods: Data on hospitalizations for acute airway changes and their complications in children <9 years old were obtained from the Database of the Brazilian Department of Public Health Informatics for the period 2015 to 2020. These data were also analyzed by macroregions of Brazil (North, Northeast, Southeast, South, and Midwest). The effect of the social distancing strategy on the increase of acute laryngitis, tracheitis, otitis media, and mastitis, as absolute and relative reductions, was calculated by analyzing the annual calculation of 2015-2019 vs 2020. Results: All the hospitalizations compared in the Unified Health System (SUS) for laryngitis and acute tracheitis and otitis media decreased, considering all states of Brazil. The largest reduction in hospitalization reduction was in the North, with -94% in 2015-2019 vs 2020 in cases of laryngitis and acute tracheitis, and in the Midwest, with - 85% in 2015-2019 vs 2020 in cases of otitis media. Conclusion: Hospitalizations for laryngitis, acute tracheitis, and acute otitis media in children <9 years old decreased between March and July 2020 in Brazil, when social distancing measures were adopted due to the COVID-19 pandemic.
Keywords:
COVID-19; Laryngitis; Otitis media; Confinement; Children; Hospitalization.
RESUMO
Objetivo: O objetivo deste estudo é avaliar o impacto do distanciamento social decorrente da Covid-19 nas internações por infecções das vias aéreas superiores (IVAS), como laringite aguda, traqueíte e otite média em crianças de 0 a 9 anos no Brasil, considerando que compartilham as mesmas formas de transmissão. Métodos: Dados sobre internações por alterações agudas das vias aéreas e suas complicações em crianças <9 anos foram obtidos do Banco de Dados do Departamento Brasileiro de Informática em Saúde Pública para o período de 2015 a 2020. Esses dados também foram analisados por macrorregiões do Brasil (Norte, Nordeste, Sudeste, Sul e Centro-Oeste). O efeito da estratégia de distanciamento social no aumento de laringite aguda, traqueíte, otite média e mastite, como reduções absolutas e relativas, foi calculado analisando o cálculo anual de 2015-2019 vs. 2020. Resultados: Todas as internações comparadas no Sistema Único de Saúde (SUS) por laringite e traqueíte aguda e otite média diminuíram, considerando todos os estados do Brasil. A maior queda na redução de internações foi na região Norte, com -94% em 2015-2019 vs. 2020 nos casos de laringite e traqueíte aguda, e no Centro-Oeste, com -85% em 2015-2019 vs. 2020 nos casos de otite média. Conclusão: As internações por laringite, traqueíte aguda e otite média aguda em crianças <9 anos diminuíram entre março e julho de 2020 no Brasil, quando medidas de distanciamento social foram adotadas devido à pandemia de Covid-19.
Palavras-chave:
COVID-19; Laringite; Otite média; Confinamento; Crianças; Hospitalização.
INTRODUCTION In March 2020, the World Health Organization (WHO) declared a pandemic caused by a new species of coronavirus, COVID-19 (coronavirus disease 2019). This outbreak of the disease began in late December 2019, when patients with viral pneumonia due to an unidentified microbial agent were reported in Wuhan, Hubei Province, China.(1) Because of this, the “UPDATE OF THE COVID-19 Strategy”, a document produced by WHO, in which guidance is provided to countries according to the epidemiological change expected with the evolution of the current pandemic, was published. Therefore, health authorities had to modify and implement some measures to restrict distance and circulation at the population level, in order to reduce exposure and prevent transmission of the virus.(2)
Upper respiratory infections (URI) are commonly found in pediatric emergency care services, mainly because they are common pathologies in acute respiratory infections in children. They present transmissibility mainly through droplets dispersed through coughing and sneezing (such as an aerosol), or even through contact of regions of the body contaminated with the airways of healthy individuals, such as hands.(3) For this reason, it is important to compare the prevalence of these diseases in a period of isolation, since the dissemination of URI often occurs in schools, daycare centers, public transportation, and other public environments, which have been closed or restricted concerning distance recommendations.
Among the most common URIs, the acute viral larynx, also known as viral croup, stands out, which consists of an inflammation of the subglottic part of the larynx during respiratory virus infection. Affection is more common in infants and preschoolers, with a higher incidence at two years of age. Its evolution varies, starting with symptoms of runny nose, fever, and cough and progressing to mild to severe obstruction and difficulty breathing. Airway persistence usually lasts 48 to 72 hours and regression occurs after five days.(3) Most cases occur in autumn and winter but can manifest during any season.(4)
Bacterial tracheitis, on the other hand, is less common, but affects soft tissues of the trachea,(5) and can also expand into subglottic structures of the larynx and upper bronchial tree.(6) The main infectious agents are bacteria.(7) Affection is more common in children during the first six years of life, with the winter and autumn period being the most prominent in cases, coinciding with seasonal viral epidemics(5,8) Symptoms include fever, stridor, cough, dyspnoea, odynophagia, or dysphagia and voice change.(9)
Another very common infection in childhood is acute otitis media (AOM), especially in the preschool period, between six months and three years of age,(10) characterized by ear pain, otorite, fever, nocturnal agitation, decreased food intake, and drowsiness.(11) It is an inflammatory process, which can be viral or bacterial and usually occurs due to a complication of upper respiratory infection (URI). The risk factors for such infection are exposure to smoke, use of bottles and pacifiers, supine position, and, mainly, care in the daycare center.(10)
Therefore, it is important to highlight that the period of the beginning of restrictive measures due to the COVID-19 pandemic in Brazil occurred in February 2020, just before the autumn of the southern hemisphere, and remained throughout the winter (from March to September), a period in which there is a higher incidence of the pathologies described above. In China, in the same period, studies showed a concomitant decrease in influenza, enterovirus, and pneumonia. Therefore, the implementation of infection control measures, including the use of masks, hand hygiene, and social distancing to prevent the spread of COVID-19, may have had a strong impact on reducing the spread of other infectious pathogens in pediatrics.(12-15) Therefore, the aim of this study is to evaluate the early impact of social distancing due to COVID-19 and hospitalizations for acute laryngitis, tracheitis, and media otitis in children aged 0 to 9 years in Brazil.
METHODS The design used was an ecological study, in which data were obtained on hospitalizations for laryngitis and otitis from the database of the Department of Informatics of the Unified Health System (DATASUS) (16) which provides the diagnosis of hospitalization for the period 2015-2020 (month by month). DATASUS presents absolute numbers of hospitalizations from the public system, obtained following the International Classification of Diseases, version 10 (ICD-10). It considers the main diagnosis in hospitalization, being able to store information with universal coverage of the Brazilian population.(17) To access the data, the links “Health Information” (TABNET) - “Epidemiological and Morbidity” (Epidemiology and Morbidity) - “Hospital Morbidity” (Hospital Morbidity), “Morbidity List” (Morbidity List), respectively for the age group from 0 to 9 years, were used. These data were also analyzed by the macroregions of Brazil (North, Northeast, Southeast, South, and Midwest), due to variations in population density, climatic variation, and socioeconomic factors, considering the continental extension of the country. The months of January to June of each year were researched since it covers the typical discharge seasons in hospitalizations for laryngitis, acute tracheitis, and otitis media, and other disorders of the middle and mastoid process. To evaluate the reliability of the report, malignant neoplasm of bone and articular cartilage was used as a comparison, since social distance measurements are not expected to have a major impact on these conditions.
As this is a search for data on a platform available online, with data fed by the single health system, without personal identification of the patient, it was not necessary to analyze and approve the Research Ethics Committee. The tool, therefore, counts on the number of hospitalizations that can be stratified according to age and location.
To evaluate the effect of pandemic containment measures about the incidence of the aforementioned diseases, absolute reduction (without and with pandemic containment measures) and relative reduction (without and with pandemic containment measures) were calculated by analyzing the subsets 2015-2019 vs 2020. Thus, two analyses were made: the first aiming at a general analysis of the panorama, observing months from January to July, and another to evaluate the effect of social distancing, with April to July. March was the cut-out month because it is the period of implementation of pandemic containment measures in Brazil in 2020 and from April the country with the most impact.(18) To ensure the quality of the collection, two independent authors reviewed the data.
The calculation of the monthly incidence of hospitalizations in the public health system used the formula total number of hospitalizations/population number per age (per year and place [Brazil-IBGE]) x 100,000 inhabitants).(19) Health insurance each year, provided by the National Health Agency, ranged from 20.80% in 2015 to 19.60% in 2020 for the population under 14 during the study period.(20) This percentage was excluded from the denominator, as the population can make use of other hospital means, and hospitalization data are not included in DATASUS. In order to calculate the difference in incidence between pandemic periods with and without containment measures, the incidence rate ratio (IRR) was used to assess statistical significance, with a 95% confidence interval.
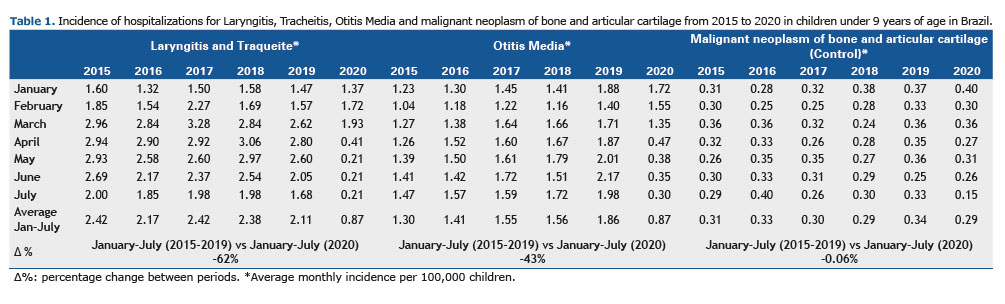
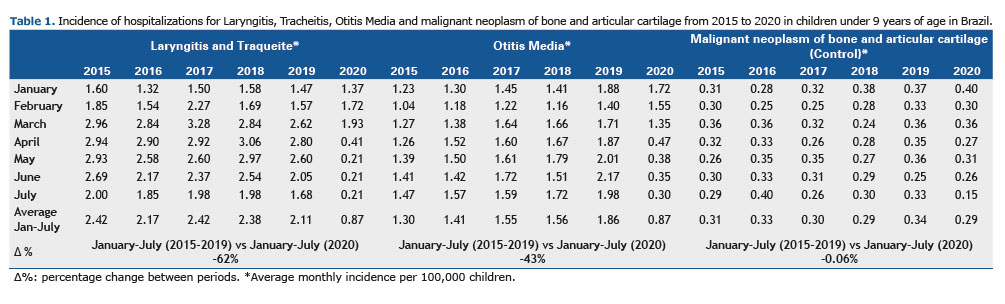
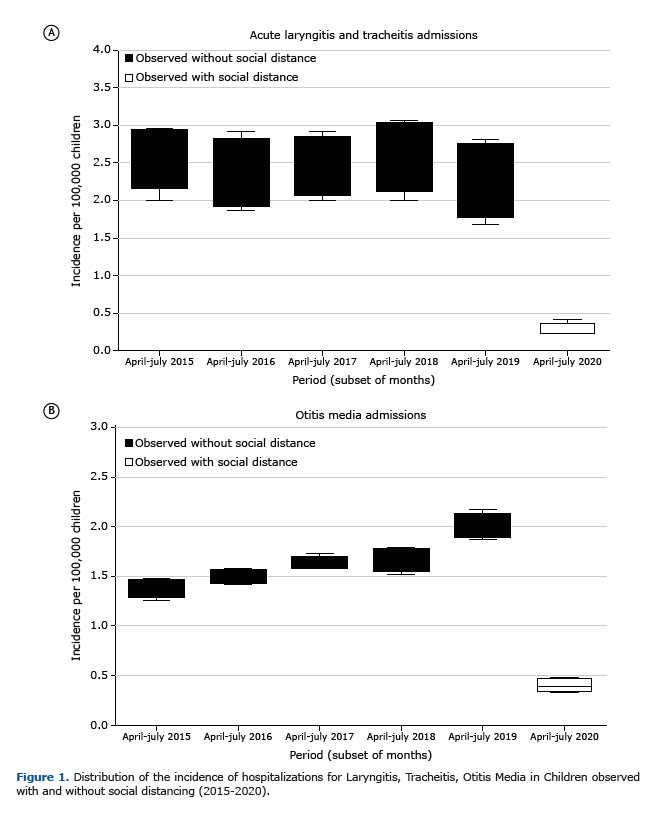
RESULTS Based on hospitalizations in the Unified Health System (SUS), through datasus information, the monthly distribution of the incidence of hospitalizations for laryngitis and acute tracheitis in January to February was similar, with a tendency to decrease over the study period. (2015-2020). The lowest incidence was observed in January 2016, with 1.32 / 100,000 hospitalizations, and the highest in February 2017, with 2.27 / 100,000 hospitalizations. In the period between March and April, the downward trend was maintained, but with peaks of hospitalizations, mainly in March 2017, with 3.28 / 100,000 hospitalizations, and April 2018, with 3.06 / 100,000 hospitalizations, with the lowest incidence recorded in this period being April 2020, with 0.41 / 100,000 hospitalizations. The month of May, during the years analyzed, remained with a linear pattern and sharp decrease in 2020. The highest incidence was 2.97 / 100,000 in 2018 and the lowest was 0.21 / 100,000 in 2020. June maintained a very close incidence in 2015, 2016, 2017, and 2018, with a fall in incidence in 2019; however, in 2020, the month of June showed a significant drop in this parameter, a drop that had been occurring since April, with 0.41 / 100,000 hospitalizations to 0.21 / 100,000 in May, June, and July. In the period between January and July 2015 to 2020, the incidence of laryngitis and acute tracheitis was 2.42 / 100,000 (2015), 2.17 / 100,000 (2016), 2.42 / 2100,000 (2017), 2.38 / 100,000 (2018), 2.11 / 100,000 (2019), 0.87 / 100,000 (2020), respectively.
Regarding the monthly distribution of the incidence of hospitalizations due to otitis media, the months from January to March presented similar values, with a tendency to increase over the period studied (2015-2020). The lowest incidence was observed in February 2015, with 1.04 /100,000 hospitalizations, and the highest in January 2019, with 1.88 / 100,000 hospitalizations. The months of April and May, during the years analyzed, maintained a linear increase, but a sharp drop in 2020. The highest incidence was 2.01 / 100,000 in 2019 and the lowest was 0.38 / 100,000 in 2020. The same pattern is observed maintained in July, with an increase in incidences from 2015 to 2019, with a higher incidence recorded in 2019, with 1.98 / 100,000, but with a sharp drop in 2020, reaching 0.30 / 100,000. In the period between January and July 2015 to 2020, the incidence of otitis media was 1.30 / 100,000 (2015), 1.41 / 100,000 (2016), 1.55 / 10 000 (2017), 1.56 / 100,000 (2018), 1.86 / 100,000 (2019), 0.87 / 100,000 (2020), respectively, as shown in Table 1.
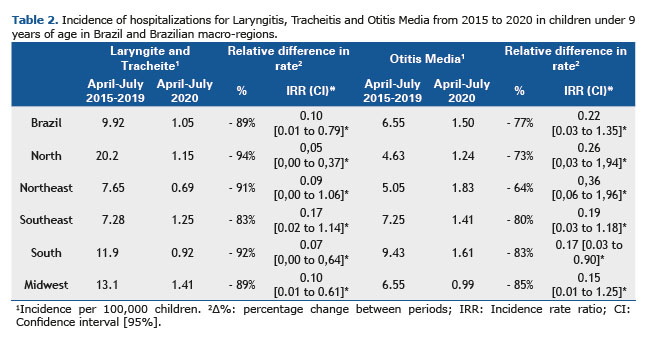
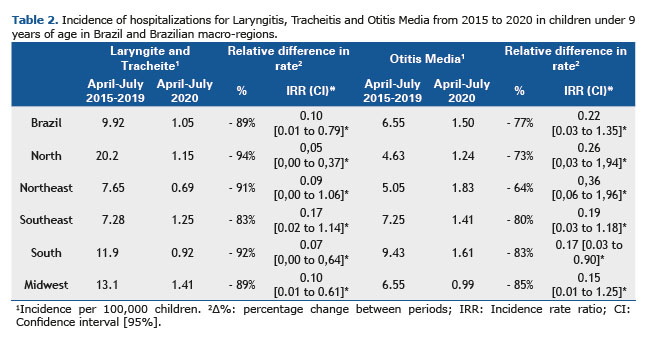
In the comparison of subsets by macroregions of Brazil on laryngitis and acute tracheitis (April to July 2015 to April to July 2020), there was also a significant reduction in all comparisons. The North region showed the largest reduction in the incidence of hospitalizations, with -94% [IRR 0.05 (0.00 to 0.37)] in 2015-2019 vs 2020. In the Northeast, the reduction ranged from - 91% [IRR 0.09 (0.00 to 1.06)] in 2015-2019 vs 2020. For the Southeast region, there was a reduction of -83% [IRR 0.17 (0.02 to 1.14)] in 2015-2019 vs 2020. The Southern region showed a reduction in incidence ranging from -92% [IRR 0.07 (0.00 to 0.64)] in 2015-2019 vs 2020. In the Midwest region, the variation was -89% [IRR 0.10 (0.01 to 0.61)] in 2015-2019 vs 2020 in the incidence of hospitalizations.
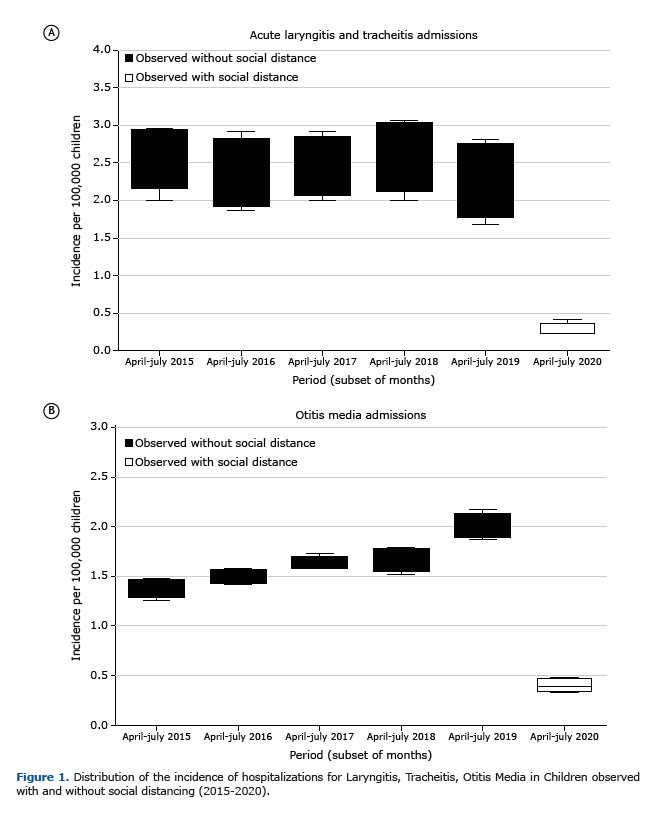
In the subsets by macroregions of Brazil, the comparison with otitis media (April to July 2015 to 2019 vs. April to July 2020), there was a significant and relevant decrease in all comparisons. In the North region, the reduction in the incidence of hospitalizations was -73% [IRR 0.26 (0.03 to 1.94)] in 2015-2019 vs 2020. In the Northeast, the reduction ranged from - 64% [IRR 0.36 (0.06 to 1.96)] in 2015-2019 vs 2020. For the Southeast region, there was a reduction of -80% [IRR 0.19 (0.03 to 1.18)] in 2015-2019 vs 2020. The Southern region showed a reduction in incidence ranging from -83% [IRR 0.17 (0.03 to 0.90)] in 2015-2019 vs 2020. The Midwest region showed the greatest variation, with -85% [IRR 0.15 (0.01 to 1.25)] in 2015-2019 vs 2020 in the incidence of hospitalizations. The absolute total number of hospitalizations, the incidence of hospitalizations per 100,000 inhabitants (0 to 9 years), and the differences between hospitalizations in the period, between 2015 and 2020, are shown in Table 2. Figure 1 summarizes the results found in this study.
Through data obtained by DATASUS and its analysis over the years in Brazil, this study aims to evaluate the impacts of measures applied to social distancing, in order to reduce the incidence of pediatric hospitalizations in children aged 0 to 9 years due to upper airway infections. Such interventions, implemented by the Brazilian Ministry of Education, to control viral spread in environments such as schools and daycare centers, for example, entered into force on March 17, near the beginning of autumn in the southern hemisphere, where there is usually a significant increase in hospitalizations for laryngitis, acute tracheitis and otitis media in the pediatric population.(4) Furthermore, because of the high population index and that the period of implementation of distance measures coincides with the period in which the causative agents of the diseases mentioned above, epidemiological data have numerous advantages in terms of quality.(21)
Considering data from the Centers for Disease Control and Prevention (CDC), an agency of the U.S. Department of Health and Human Services, hospitalizations for COVID-19 in the pediatric population are extremely unusual, with about 4.1%. These data decrease even more when it comes to the need for a pediatric intensive care unit (IU) for individuals of the same age group, with less than 1%. Such rates have also been observed in other developed countries, such as China, Italy, France, and Spain, which maintain a very similar pattern. In France, for example, François Angoulvant, a pediatric emergency physician, collected information on visits to six emergency rooms of children in Paris from March 2020, when the French government ordered the partial closure of the region on account of the arrival of COVID-19. Data from 871,500 patients between 2017 and 2020 were analyzed, in which hospitalizations in pediatric emergency rooms decreased by 45% during the months of the pandemic.(22) Brazil, in turn, presented, through a recent study, 56% of hospital admissions being in the pediatric population, among which 19% required PICUs in cases of COVID-19; however, this study analyzed reference hospitals of high clinical complexity and, therefore, that obtained patients with multiple comorbidities, which may be the reason for such a sharp deviation when compared to studies in more developed countries. Although a 2020 Hoang et al.systematic review identified co-infection in 6% of cases of pediatric hospitalization with Mycoplasma pneumonia and Respiratory Sincicial Virus, many studies point to a significant decrease in several regions of the world in dealing with the diseases mentioned and their respective hospitalizations in pediatrics.(23) The study Yeoh et al.(24)) analyzed the pediatric population of Australia and showed reductions of 98.0% and 99.4% in RSV and influenza detections, respectively, until the winter of 2020; as well as a study conducted in Belgium showed a decrease of >99% in the recorded cases of RSV in 2020 compared to previous years.(25) This fact may be closely linked because the transmissibility of respiratory agents decreased due to isolation measures, with a general awareness of the need for proper handwashing, use of alcohol gel, regular cleaning of toys, individual use of utensils and personal masks, in addition to the closure of schools and sports clubs proposed by the Brazilian government.(26,27) Therefore, all the measures mentioned may have contributed to the reduction of laryngitis, tracheitis, and acute otitis media in children, reducing interpersonal contact and greater care for personal hygiene.
According to the Brazilian Society of Pediatrics, it is necessary to have careful maintenance of care for children and adolescents even in times of pandemics. According to data from FIOCRUZ - the main non-university institution for the training and qualification of human resources for the SUS and the area of science and technology in Brazil(28) - in 2020 some health units recorded a reduction in the number of outpatient care of up to 90% between March and July 2020, when compared to the same period in 2019, causing several losses to the patient and future overcrowding in the country’s health services.(23) This fact was also analyzed through a recent multicenter study, which showed that emergency visits and hospital admissions were greatly reduced during COVID-19 blockades in the Netherlands, as in the rest of the world, especially for children with transmissible infections.(29) Although it is widely known that this period of isolation has brought health problems when it comes to routine visits or monitoring of chronic diseases, it is possible to note that the measures proposed by the guidelines for the control of transmission of SARS -CoV-2 infection have had an impact on other etiological agents, which are related to pediatric laryngitis, acute tracheitis and otitis media due to the forms of contagion.(27,30,31) That is, although this factor can be seen as confounding, it cannot be said as a direct or isolated influence on the results found in our study, because, as observed in previous studies, our main hypothesis is that non-pharmacological health measures to contain the COVID-19 pandemic have a significant impact on the spread of several respiratory viruses that still have a lower propagation potential than SARS-CoV-2.
There was a sharp decrease in hospitalization rates between March and July 2020 in all Brazilian macro-regions, during which restrictive measures were implemented.(2) Our findings show that, annually, the incidence of hospitalizations for laryngitis, acute tracheitis, and otitis media increases, as occurs in countries in other developing countries, such as Brazil. However, it is noted that there was a drastic reduction in the incidence of pediatric hospitalizations for upper airway infections in the period from 2015-19 to 2020 from March when in Brazil social distancing due to COVID-19 began. Before this period, that is, in January and February 2020, there was a similar incidence over the years, with an exponential increase in hospitalization cases considering the seasonality of the disease in the country.(32) For hospitalizations for laryngitis and acute tracheitis, the data suggest a downward trend over the study period (2015-2020). The lowest incidence occurred in April 2020, and this significant reduction was maintained in May and June. In hospitalizations for acute otitis media, there was an upward trend in the period from 2015 to 2020. The months of January to March maintained similar values, but from April to July, the increase observed until 2019 was interrupted by a sharp drop in the year 2020. In the comparison between the Brazilian macroregions, the North region showed a greater reduction in hospitalizations for laryngitis and acute tracheitis (-94%). Secondly, the South region decreased -92%, followed by the Northeast (-91%), Midwest (-89%), and Southeast (-83%). As for hospitalizations due to acute otitis media, there was a marked decrease in all the comparations, the most significant in the Midwest region (-85%). The South region fell -83% and was followed by the Southeast (-80%), North (-73%), and Northeast (-64%).
Finally, the present retrospective study, however, has some limitations, such as the impossibility of evaluating isolated non-pharmacological interventions, because they were implemented simultaneously. In terms of data collection, another limitation is about the platform, because they were filled out by third parties, DATASUS employees, and not by the researchers who wrote it, considering the pandemic period and social distance. Data were collected for each month with a delay of two months and, according to our previous experiences, this period is sufficient for DATASUS to update the final numbers or the very approximate values, considering that the data are included according to the forms of Hospitalization Authorizations, in Brazil AIH (Hospital Admission Authorization). Still in this regard, the data present population nature, with robust national and regional epidemiological information, taking into account the population size, which reiterates the findings and presents as an advantage concerning the other studies.(33,34) Moreover, when analyzing hospitalizations for otitis, we are only covering severe cases, considering that the mildest and most common cases receive outpatient treatment, which may represent a bias in terms of estimating the real fall in the incidence of this infection. However, and there are such limitations, we consider that these results truly reflect the current moment, considering that these were the same throughout the evaluation period, which reinforces the validity of the main findings of the present study. Such changes in the profile of pediatric hospitalizations, in terms of epidemiology, had not been reported before in Brazil.
ACKNOWLEDGMENTS The authors would like to thank the Brazilian Health Institutions that develop a DATASUS database and make it available for research: Department of Informatics of the Unified Health System and Ministry of Health.
AUTHOR CONTRIBUTIONS CRJ participated in the study planning, coordinated data collection and wrote the article. AASR, ASM, ACA, FBM, SMF, LCSM participated in the planning, data collection and writing of the first version of the paper. Frederico Friedrich participated in the analysis and final writing of the article. LAP coordinated the study planning, data collection and final writing of the article.
REFERENCES 1. WHO: World Health Organization [Internet]. WHO Director-General’s opening remarks at the media briefing on COVID-19. Switzerland: WHO; 2020 [cited 2020 Nov 5]. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
2. WHO: World Health Organization [Internet]. COVID19 strategy update. Switzerland: WHO; 2020 [cited 2020 Nov 5]. Available from: https://www.who.int/publications/i/item/covid-19-strategy-update---14-april-2020
3. Pitrez Paulo MC, Pitrez José LB. Acute upper airway infections: diagnosis and outpatient treatment. J Pediatr J River. [serial on the Internet]. 2003 June [cited 2020 Oct 21];79(Suppl 1):S77-86. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0021-75572003000700009&lng=en
4. SBP: Sociedade Brasileira de Pediatria [Internet]. Crupe viral e bacteriano. Guia Prático de Conduta. Departamento de Emergências; 2017 [cited 2020 Oct 24]. p. 1-9. Available from: https://www.sbp.com.br/fileadmin/user_upload/2017/01/Emergncia-Crupe-Viral-e-Bacteriano.pdf
5. Jones R, Santos JI, Overall JC Jr. Bacterial tracheitis. JAMA. 1979;242(8):721-6. http://dx.doi.org/10.1001/jama.1979.03300080019018. PMid:379379.
6. Conley SF, Beste DJ, Hoffmann RG. Measles-associated bacterial tracheitis. Pediatr Infect Dis J. 1993;12(5):414-5. http://dx.doi.org/10.1097/00006454-199305000-00017. PMid:8327305.
7. Hjuler IM, Hansen MB, Olsen B, Renneberg J. Bacterial colonization of the larynx and trachea in healthy children. Acta Paediatr. 1995;84(5):566-8. http://dx.doi.org/10.1111/j.1651-2227.1995.tb13696.x. PMid:7633155.
8. Wood CR. Bacterial tracheitis in children: clinical characteristics and diagnosis [Internet]. UpToDate; 2019 [cited 2020 Oct 6]. Available from: https://www.uptodate.com/contents/bacterial-tracheitis-in-children-clinical-features-and-diagnosis?search=traqueite%20acute&source=search_result&selectedTitle=1~18&usage_type=default&display_rank=1#H23
9. Casazza G, Graham ME, Nelson D, Chaulk D, Sandweiss D, Meier J. Pediatric bacterial tracheitis-a variable entity: case series with literature review. Otolaryngol Head Neck Surg. 2019;160(3):546-9. http://dx.doi.org/10.1177/0194599818808774. PMid:30348058.
10. Di Francesco RC, Moricz RD, Marone S. Otite média aguda em pediatria: diagnóstico e tratamento. Boletim da Sociedade de Pediatria de São Paulo [serial on the Internet]. 2016 [cited 2020 Oct 28];1(3):4-6. Available from: https://www.spsp.org.br/site/asp/boletins/AT3.pdf
11. Venekamp RP, Damoiseaux RA, Schilder AG. Acute otitis media in children. BMJ Clin Evid. 2014. [cited 2014 Sep 16];09:301. PMID: 25229555. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4166866/pdf/2014-0301.pdf.
12. Friedrich F, Ongaratto R, Scotta MC, Veras TN, Stein RT, Lumertz MS, et al. Early Impact of social distancing in response to Coronavirus Disease 2019 on hospitalizations for acute bronchiolitis in infants in Brazil. Clin Infect Dis. 2021;72(12):2071-5. http://dx.doi.org/10.1093/cid/ciaa1458. PMid:32986818.
13. Edwards KM. The impact of social distancing for SARS-CoV-2 on respiratory syncytial virus and Influenza Burden. Clin Infect Dis. 2020;72(12):2076-8. http://dx.doi.org/10.1093/cid/ciaa1543.
14. Fong MW, Gao H, Wong JY, Xiao J, Shiu EYC, Ryu S, et al. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings-social distancing measures. Emerg Infect Dis. 2020;26(5):976-84. http://dx.doi.org/10.3201/eid2605.190995. PMid:32027585.
15. Varela FH, Scotta MC, Polese-Bonatto M, Sartor ITS, Ferreira CF, Fernandes IR, et al. Absence of detection of RSV and influenza during the COVID-19 pandemic in a Brazilian cohort: likely role of lower transmission in the community. J Glob Health. 2021;11:05007. http://dx.doi.org/10.7189/JOGH.11.05007. PMid:33791096.
16. Brazil. DATASUS: Ministry of Health. Health Information (TABNET). [cited 2020 Jun 23]. Available at: https://datasus.saude.gov.br/informacoes-de-saude-tabnet/.
17. Sousa AF, Stadulni ARP, Costa LBA. Uso de dados do departamento de informática do Sistema Único de Saúde (DATASUS) em pesquisas científicas. Rev Multidiscip Núcleo do Conhecimento. 2021;11:171-85. http://dx.doi.org/10.32749/nucleodoconhecimento.com.br/saude/saude-datasus
18. Brasil. Lei nº 13.979, de 6 de Fevereiro de 2020. Dispõe sobre as medidas para enfrentamento da emergência de saúde pública de importância internacional decorrente do coronavírus responsável pelo surto de 2019. Diário Oficial da União; Brasília; 2020.
19. IBGE: Instituto Brasileiro de Geografia e Estatística [Internet]. Projeções da população. Rio de Janeiro: IBGE; 2018 [cited 2020 June 8]. Available from: https://www.ibge.gov.br/estatisticas/sociais/populacao/9109-projecao-da-populacao.html?edicao=21830&t=resultados
20. Brazil. ANS: National Supplementary Health Agency. TABNET [Internet]. [cited 2020 Jun 23]. Available from: https://www.gov.br/ans/pt-br.
21. Brasil. Ministério da Educação. Portaria nº 343, de 17 de Março de 2020. Dispõe sobre a substituição das aulas presenciais por aulas em meios digitais enquanto durar a situação de pandemia do Novo Coronavírus - COVID-19 [Internet]. Diário Oficial da União; Brasília; 2020 [cited 2021 Jan 18]. Available from: https://www.in.gov.br/en/web/dou/-/portaria-n-343-de-17-de-marco-de-2020-248564376
22. Angoulvant F, Ouldali N, Yang DD, Filser M, Gajdos V, Rybak A, et al. COVID-19 pandemic: Impact caused by school closure and national blockade on pediatric visits and hospitalizations for viral and non-viral infections, a time series analysis. Clin Infect Dis. 2020 Jun 3:ciaa710. PMID: 33501967.
23. Instituto Fernandes Figureira. COVID-19 e saúde da criança e do adolescente [Internet]. Rio de Janeiro: IFF; 2020 [cited 2021 Jan 20]. p. 1-70. Available from: http://www.iff.fiocruz.br/pdf/covid19_saude_crianca_adolescente.pdf
24. Yeoh DK, Foley DA, Minney-Smith CA, Martin AC, Mace AO, Sikazwe CT, et al. The impact of COVID-19 public health measures on detections of influenza and respiratory syncytial virus in children during the 2020 Australian winter. Clin Infect Dis. 2021;72(12):2199-202. http://dx.doi.org/10.1093/cid/ciaa1475. PMid:32986804.
25. Van Brusselen B, De Troeyer K, ter Haar E, Auwera AV, Poschet K, Van Nuijs S, et al. Bronchiolitis in COVID-19 times: a nearly absent disease? Eur J Pediatr. 2021;180:1969-73. http://dx.doi.org/10.1007/s00431-021-03968-6.
26. Brasil. Ministério da Saúde. Saúde anuncia orientações para evitar a disseminação do coronavírus [Internet]. Brasília: Ministério da Saúde; 2020 [cited 2021 Jan 31]. Available from: https://www.gov.br/saude/pt-br/assuntos/noticias/saude-anuncia-orientacoes-para-evitar-a-disseminacao-do-coronavirus
27. Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM, et al. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014;134(5):e1474-502. http://dx.doi.org/10.1542/peds.2014-2742. PMid:25349312.
28. Fiocruz: Fundação Oswaldo Cruz. Pesquisa e ensino [Internet]. 2021 [cited 2021 Jan 18]. Available from: https://portal.fiocruz.br/pesquisa-e-ensino#:~:text=A%20Fiocruz%20%C3%20%20main,e%20v%C3%A1rios%20programs%20lato%20sensu
29. Kruizinga MD, Peeters D, van Veen M, van Houten M, Wieringa J, Noordzij JG, et al. The impact of lockdown on pediatric ED visits and hospital admissions during the COVID19 pandemic: a multicenter analysis and review of the literature. Eur J Pediatr. 2021;180(7):2271-9. http://dx.doi.org/10.1007/s00431-021-04015-0. PMid:33723971.
30. Angoulvant F, Ouldali N, Yang DD, Filser M, Gajdos V, Rybak A, et al. Coronavirus Disease 2019 Pandemic: Impact caused by school closure and national lockdown on pediatric visits and admissions for viral and nonviral infections - a time series analysis. Clin Infect Dis. 2021;72(2):319-22. http://dx.doi.org/10.1093/cid/ciaa710. PMid:33501967.
31. Erlichman M, Zalut T, Schwartz S, Weiser G. The ongoing indirect effect of the COVID 19 pandemic on a pediatric emergency department. PLoS One. 2021;16(5):e0251003. http://dx.doi.org/10.1371/journal.pone.0251003.
32. Pedreira BAM. Fatores de risco para hospitalização por infecção respiratória aguda em crianças [Internet]. Salvador: Universidade Federal da Bahia; 2013 [cited 2021 Jan 18]. Available from: https://repositorio.ufba.br/ri/bitstream/ri/12830/1/DISS.%20BETANIA%202013.pdf
33. Friedrich F, Valadão MC, Brum M, Comaru T, Pitrez PM, Jones MH, et al. Impact of maternal dTpa vaccination on the incidence of pertussis in young infants. PLoS One. 2020;15(1):e0228022. http://dx.doi.org/10.1371/journal.pone.0228022.
34. Scotta MC, Veras TN, Klein PC, Tronco V, Polack FP, Mattiello R, et al. Impact of 10-valent pneumococcal non-typeable Haemophilus influenzae protein D conjugate vaccine (PHiD-CV) on childhood pneumonia hospitalizations in Brazil two years after introduction. Vaccine. 2014;32(35):4495-9. http://dx.doi.org/10.1016/j.vaccine.2014.06.042. PMid:24958703.