ABSTRACT
The treatment of COPD has become increasingly effective. Measures that range from behavioral changes, reduction in exposure to risk factors, education about the disease and its course, rehabilitation, oxygen therapy, management of comorbidities, and surgical and pharmacological treatments to end-of-life care allow health professionals to provide a personalized and effective therapy. The pharmacological treatment of COPD is one of the cornerstones of COPD management, and there have been many advances in this area in recent years. Given the greater availability of drugs and therapeutic combinations, it has become increasingly challenging to know the indications for, limitations of, and potential risks and benefits of each treatment modality. In order to critically evaluate recent evidence and systematize the major questions regarding the pharmacological treatment of COPD, 24 specialists from all over Brazil gathered to develop the present recommendations. A visual guide was developed for the classification and treatment of COPD, both of which were adapted to fit the situation in Brazil. Ten questions were selected on the basis of their relevance in clinical practice. They address the classification, definitions, treatment, and evidence available for each drug or drug combination. Each question was answered by two specialists, and then the answers were consolidated in two phases: review and consensus by all participants. The questions answered are practical questions and help select from among the many options the best treatment for each patient and his/her peculiarities.
Keywords:
Pulmonary disease, chronic obstructive/drug therapy; pulmonary disease, chronic obstructive/prevention & control; pulmonary disease, chronic obstructive/therapy.
RESUMO
O tratamento da DPOC vem se tornando cada vez mais eficaz. Medidas que envolvem desde mudanças comportamentais, redução de exposições a fatores de risco, educação sobre a doença e seu curso, reabilitação, oxigenoterapia, manejo de comorbidades, tratamentos cirúrgicos e farmacológicos até os cuidados de fim de vida permitem ao profissional oferecer uma terapêutica personalizada e efetiva. O tratamento farmacológico da DPOC constitui um dos principais pilares desse manejo, e muitos avanços têm sido atingidos na área nos últimos anos. Com a maior disponibilidade de medicações e combinações terapêuticas fica cada vez mais desafiador conhecer as indicações, limitações, potenciais riscos e benefícios de cada tratamento. Com o intuito de avaliar criticamente a evidência recente e sistematizar as principais dúvidas referentes ao tratamento farmacológico da DPOC, foram reunidos 24 especialistas de todo o Brasil para elaborar a presente recomendação. Foi elaborado um guia visual para a classificação e tratamento adaptados à nossa realidade. Dez perguntas foram selecionadas pela relevância na prática clínica. Abordam a classificação, definições, tratamento e evidências disponíveis para cada medicação ou combinação. Cada pergunta foi respondida por dois especialistas e depois consolidadas em duas fases: revisão e consenso entre todos os participantes. As questões respondidas são dúvidas práticas e ajudam a selecionar qual o melhor tratamento, entre as muitas opções, para cada paciente com suas particularidades.
Palavras-chave:
Doença pulmonar obstrutiva crônica/tratamento farmacológico; Doença pulmonar obstrutiva crônica/prevenção & controle; Doença pulmonar obstrutiva crônica/ terapia.
INTRODUCTIONThe treatment of COPD has become increasingly effective. Measures that range from behavioral changes, reduction in exposure to risk factors, education about the disease and its course, rehabilitation, oxygen therapy, management of comorbidities, and surgical and pharmacological treatments to end-of-life care allow health professionals to provide a personalized and effective therapy. However, having accurate knowledge of the indications for, limitations of, and potential risks and benefits of each treatment modality has become a challenge. This challenge is even more acute when we have to adapt evidence in the literature to fit the peculiarities of our country, given the frequent challenges faced in both public and private clinical practice.
The pharmacological treatment of COPD is one of the cornerstones of COPD management, and there have been many advances in this area in recent years.(1) In 2011, a systematic review of the advances in the pharmacological treatment of COPD was published in the JBP. It is striking the extent to which the knowledge of and the resources available to treat COPD have evolved since then.(2)
The individualization of treatment is essential and should be based on the availability of existing drugs, disease severity, patient preferences, drug interactions, and comorbidities. The goal should always be to meet the disease control objectives effectively. In order to critically evaluate recent evidence and systematize the major questions regarding the pharmacological treatment of COPD, specialists from all over Brazil gathered to develop the present recommendations.
It is always important to emphasize that the pharmacological treatment of COPD should be complemented by measures such as smoking cessation, encouragement for physical activity, pulmonary rehabilitation, and vaccination to prevent viral infections and pneumonia, as well as by measures against advanced disease, such as oxygen therapy, surgical treatment, endoscopic treatment, and lung transplantation.(3) These treatment measures should always be considered and, when indicated, should be implemented together with the appropriate drug therapy.(4)
Chart 1 shows the major drugs available for the treatment of COPD, and Chart 2 serves as a guide for the classification and treatment of COPD, both of which were adapted to fit the situation in Brazil. The 10 questions answered in the present recommendations are practical questions and help select from among the many options the best treatment for each COPD patient.

 1. HOW SHOULD COPD SEVERITY BE CLASSIFIED?
1. HOW SHOULD COPD SEVERITY BE CLASSIFIED? The first international consensus guidelines on COPD used the degree of FEV1 impairment for determining disease severity. Current guidelines, however, combine assessment of symptoms and exacerbations of COPD (ECOPD) with spirometry results to classify disease severity, acknowledging that spirometric measurements alone are insufficient. In fact, dyspnea intensity and impaired health status correlate poorly with FEV1.(5)
The classification of COPD severity is aimed at determining the degree of airflow obstruction, determining symptom intensity (specifically the degree of dyspnea), and evaluating the risk of ECOPD.
DyspneaDyspnea is the major factor responsible for the development of disability in COPD. Patients who have the same degree of airflow obstruction can exhibit different degrees of dyspnea.(6) The modified Medical Research Council (mMRC) dyspnea scale is easy to administer, expresses the intensity of the impact of the symptom, and predicts 5-year survival.(7) Chart 3 shows an adapted version of the mMRC dyspnea scale for use in Brazil. It is important to question patients with COPD about the time of day they most often experience dyspnea so that it is possible to adapt their daily lives to their degree of dyspnea. A shorter-acting drug may eventually provide more benefits for patients who most often experience dyspnea in the morning.(8)
 Questionnaire on health status in COPD
Questionnaire on health status in COPDDyspnea is not the only symptom of COPD. COPD impacts health status for several reasons that are not quantified in assessment of dyspnea in isolation. Quality of life questionnaires are quite important for evaluating the efficacy of treatments but are impractical for use in routine practice.
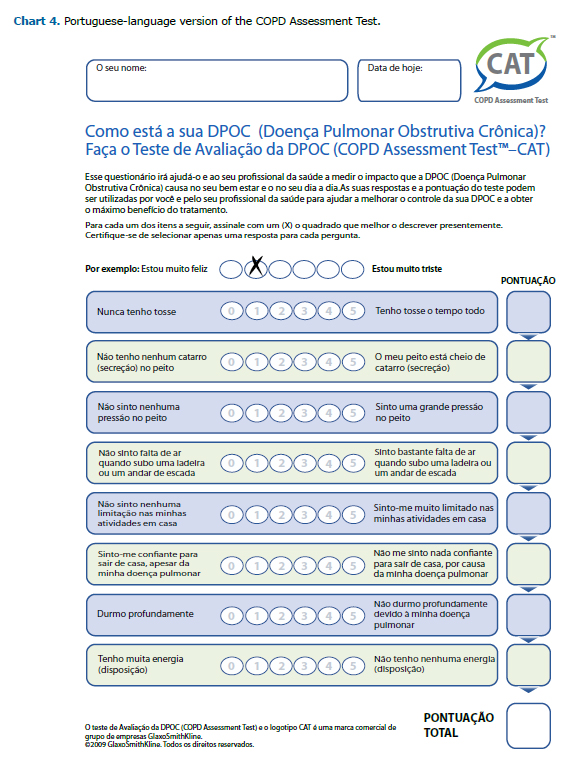
To fill the need for an easy-to-administer instrument that assessed health status multidimensionally and had an impact on the evaluation and follow-up of COPD, several questionnaires have been developed, the most widely used of which is the COPD Assessment Test (CAT). Chart 4 shows the Portuguese-language version of the CAT, with its questions and scoring system.(9) The CAT correlates well with quality of life questionnaires, FEV1, and dyspnea as measured by the mMRC dyspnea scale. In addition, the CAT provides complementary information on issues such as cough, expectoration, sleep, and vitality, among others that are not addressed in traditional assessments.(10-12)
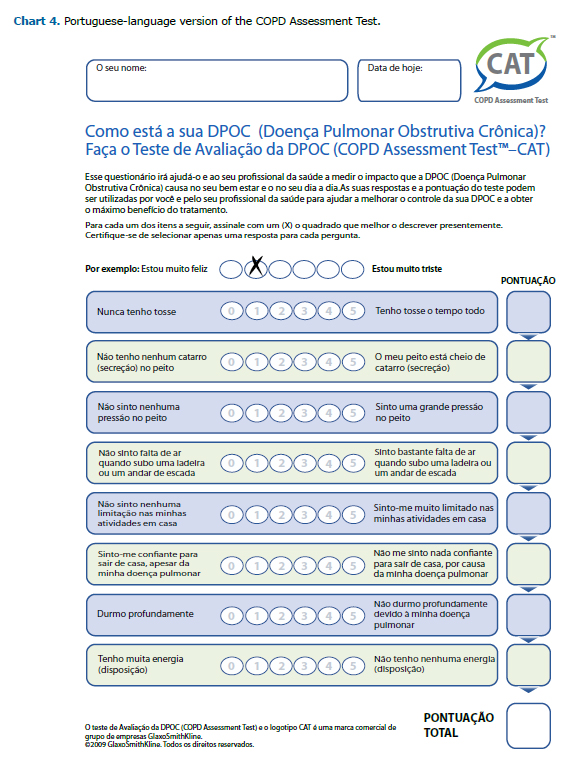
For the proposed classification (Chart 2), a CAT score ≥ 10 (Chart 4) distinguishes patients with COPD who are highly asymptomatic from those who are mildly asymptomatic and should be used, together with mMRC dyspnea scale scores (Chart 3) and pulmonary function results, to determine disease severity.
FEV1
FEV1 is the simplest measure of the degree of airway obstruction in COPD. A reduced FEV1 is associated with increased mortality in COPD, in addition to its role in identifying the disease and classifying disease severity. FEV1 is also associated with quality of life in patients with COPD.(13-15) Although FEV1 does not reflect all domains of the disease, its use, in combination with assessment of dyspnea intensity with the mMRC dyspnea scale, is simple and applicable to the care provided by general practitioners and specialists.(16-19)
The classification of COPD severity proposed by the Brazilian Thoracic Association uses post-bronchodilator FEV1 values (expressed as percent of predicted value) and mMRC dyspnea scale scores (Chart 3) or CAT scores (Chart 4). The worst-result criterion should be used. COPD should be classified as mild, moderate, severe, or very severe, and treatment should be recommended for each severity class (Chart 2).
2. WHAT IS A COPD EXACERBATOR? ARE THERE DIFFERENCES IN PROGNOSIS AND TREATMENT? Several definitions exist for ECOPD in the literature. About 30 years ago, Anthonisen et al.(20) defined ECOPD as the presence of at least two of the following changes: increased dyspnea; increased expectoration; and increased sputum purulence. These criteria are still used. ECOPD are events in the natural course of the disease characterized by a sustained worsening of the patient's usual respiratory symptoms that is beyond normal day-to-day variations and warrants a change in regular medication.(21)
Although ECOPD can be caused by several factors, most are associated with viral or bacterial infections. More than 40% of ECOPD are related to respiratory viruses, but non-infectious agents that irritate the airways, such as air pollution, can also be triggering factors.(22)
ECOPD increase the inflammatory process, accelerate disease progression, worsen quality of life, and increase the risk of recurrent ECOPD and hospitalizations that may lead to the death of patients. ECOPD are also associated with an increased risk of cardiovascular events, especially acute myocardial infarction.(22,23)
In-hospital mortality during ECOPD ranges from 3.6% to 11%; the risk of hospitalization can increase by 23% to 43% during the year following hospitalization; among ICU patients, in-hospital mortality is 24% and can be as high as 42% after 1 year; and the calculated fatality rate (excess mortality compared with stable COPD) is 15.6%, which underscores the importance of measures to prevent and treat ECOPD.(17,24)
Risk factors for frequent ECOPD include advanced age, very compromised pulmonary function, cough with expectoration, comorbidities, gastroesophageal reflux disease, and, in particular, a history of ECOPD.(25)
A study(26) that followed 2,138 treated patients with COPD over 3 years found that the major predictor of ECOPD was a history of ECOPD in the preceding year (OR = 4.30; 95% CI: 3.58-5.17) and that the exacerbator phenotype was generally maintained in the following years of follow-up. Exacerbators are a distinct group of patients, and being an exacerbator is unrelated to disease severity. In that same study, among patients with moderate COPD as defined by spirometry (FEV1 between 50% and 80%), there were 22% of exacerbators.(26)
Based on morbidity and prognosis studies, frequent exacerbators were defined as patients with COPD who experience two or more ECOPD over a 1-year period, each at least 4 weeks apart after the end of the treatment of a previous ECOPD or 6 weeks apart, beginning at the event onset, in untreated cases.(4) Patients who experienced an ECOPD requiring hospitalization in the preceding 12 months should also be treated as exacerbators.
The relationship observed between ECOPD and worsened prognosis in several studies warrants that special attention that exacerbators should be given with regard to the maintenance pharmacological treatment of COPD.(24,27-30) One of the goals of the present recommendations was to separate the pharmacological treatment of exacerbators from that of non-exacerbators. Both treatments depend on pulmonary function results for definition of the most appropriate drugs (Chart 2).
3. WHAT ARE THE GOALS OF THE PHARMACOLOGICAL TREATMENT OF COPD? The goals of the pharmacological treatment of COPD are to reduce symptoms, which includes relieving dyspnea and cough; to improve health status and exercise tolerance; to reduce risk, which includes mitigating disease progression; to prevent and treat ECOPD; and to reduce mortality.
The choice of the most appropriate treatment should take into account symptom intensity, ECOPD, adverse effects, comorbidities, cognitive changes, adaptation to the device, and drug availability and costs. Therefore, pharmacological treatment should be individualized, there being drug options suited to each patient's profile. However, some general considerations should be made to avoid inappropriate or excessive drug use.(4)
In patients who are at low risk of ECOPD and are mildly asymptomatic, the first consideration to be made is whether maintenance treatment is required. The evidence regarding this specific profile will be discussed later. If the decision is for symptomatic treatment, patients can be started on an inhaled long-acting bronchodilator alone, no class being preferred in the choice. Long-acting β2 agonists (LABAs) and long-acting antimuscarinic agents (LAMAs) are options. Long-acting bronchodilators are more effective than short-acting bronchodilators and should be prioritized in the treatment of patients with persistent symptoms. If symptoms remain despite initial treatment, a LABA/LAMA combination should be prescribed.(31,32)
In patients with more severe dyspnea but at low risk of ECOPD, dual LABA/LAMA bronchodilation therapy is indicated, always taking into account availability, side effects, and individual response. Inhaled corticosteroids (ICSs) are rarely indicated for patients at low risk of ECOPD; ICSs should be added to the treatment when both COPD and asthma are present.(33)
Exacerbators who are mildly asymptomatic and have no severe functional limitation (FEV1 > 50%) can be initially treated with a long-acting bronchodilator alone. In such cases, LAMAs are superior to LABAs in preventing ECOPD.(34)
For exacerbators who are more symptomatic or have more severe functional limitation, treatment can be initiated with a LABA/LAMA combination or, if the patient is already using such a combination, an ICS can be added, constituting triple therapy.
An ICS, always in combination with a LABA, is indicated in selected patients. LABA/ICS combinations are indicated in patients with specific phenotypes, such as those with asthma and COPD or with blood or sputum eosinophilia. The indications for LABA/ICS combination therapy will be discussed later.
There are as yet no studies to determine whether triple therapy is superior to LABA/LAMA combination therapy in preventing ECOPD. As previously mentioned, patients with asthma and COPD should always be treated with ICSs, irrespective of the number of ECOPD.(33) For patients who continue to have ECOPD despite triple therapy, there are second- and third-line options for preventing ECOPD that will be discussed later.
4. WHAT SHOULD BE THE PHARMACOLOGICAL TREATMENT FOR MILD COPD (FEV1 > 80% OF PREDICTED AND MMRC SCALE SCORES ≤ 1)? Patients with mild COPD have structural changes in the airways and lung parenchyma, as well as several physiological changes. However, there is no evidence of clinical importance of these changes in asymptomatic patients. In one study,(35) in which 519 individuals with an FEV1/FVC ratio < 0.70 and an FEV1 > 80% of predicted were followed, 56.8% of those patients had no respiratory symptoms. Multivariate adjusted analysis showed that there were no differences between asymptomatic patients and the reference group (asymptomatic patients with normal pulmonary function test results) regarding health care utilization or quality of life.(35) The presence of symptoms was one of the best predictors of health care utilization in those with mild obstruction.(35-38) In that group, 3 years of treatment with budesonide did not affect the rate of decline in FEV1 or respiratory symptoms, including ECOPD.(35-38)
It has been demonstrated that dynamic hyperinflation occurs even in patients with mild-to-moderate disease. Treatment with tiotropium improved dynamic hyperinflation in patients with moderate disease but not in those with mild disease. It was also demonstrated that 6 weeks of treatment with tiotropium modestly improved inspiratory capacity in those patients but had no effect on exercise tolerance.(39) In another study, there was improvement in airflow limitation.(40)
The Global Initiative for Chronic Obstructive Lung Disease recommends the use of a short- or long-acting bronchodilator to relieve dyspnea,(4) which does not apply to patients with mild COPD and an mMRC score ≤ 1 (Chart 3).(9) There is no evidence of benefit of pharmacotherapy for other outcomes.(5,10) In summary, although pharmacological therapy has effects on some physiological changes, to date, there have been no studies on which to base a recommendation for the use of this form of therapy in asymptomatic patients with mild COPD. If the symptoms are considered relevant, short- or long-acting bronchodilators can be used depending on patient preference and can be continued depending on symptom improvement. As symptoms become more prominent and frequent or ECOPD occur, the option should be for a long-acting bronchodilator.(4)
5. DOES A LABA/LAMA COMBINATION PROVIDE GREATER BENEFITS THAN LABA OR LAMA MONOTHERAPY IN PATIENTS WITH COPD? Bronchodilators are the cornerstone of COPD treatment. The addition of a second long-acting bronchodilator as a different mechanism of action increases the benefits for various outcomes, especially dyspnea and the frequency and severity of ECOPD. LABA/LAMA combinations are indicated in symptomatic patients with moderate-to-very-severe COPD and in exacerbators.(4)
A study conducted in Brazil and involving patients who remained symptomatic despite treatment with salmeterol showed that the addition of tiotropium was able to improve pulmonary function, decrease dyspnea during physical activity, and improve performance in activities of daily living within 2 weeks.(41)
ExacerbationsOnly one study has been aimed primarily at evaluating the effect of a LABA/LAMA combination vs. monotherapy on ECOPD, and it demonstrated that indacaterol/glycopyrronium decreased the annual rate of moderate or severe ECOPD and the rate of all ECOPD, including mild ones, and increased morning pre-dose FEV1 relative to glycopyrronium alone.(42)
Comparisons of umeclidinium/vilanterol for 24 weeks vs. umeclidinium, vilanterol, or tiotropium alone found no differences in the time to first ECOPD. Those studies, however, were not designed to assess ECOPD as a primary outcome.(43,44) Likewise, comparisons of aclidinium/formoterol vs. either monotherapy in 24-week studies, which were also not designed to assess ECOPD, showed no significant differences in the rate of ECOPD.(45,46)
Tiotropium/odolaterol is still being studied regarding the frequency of ECOPD. In a recent study, tiotropium/odolaterol was superior to either monotherapy in improving FEV1, dyspnea, hyperinflation, and rescue medication use. The improvement, although statistically significant, was below the minimal clinically important difference (MCID).(47)
DyspneaDyspnea is the most common complaint of patients with COPD. The most common assessment tool is the Transition Dyspnea Index (TDI), which considers an MCID of 1 point. Most studies assess dyspnea as a secondary outcome. A 6-week study assessed dyspnea as a primary outcome, comparing glycopyrronium/indacaterol vs. placebo or tiotropium alone.(48) A 26-week study, in which dyspnea was a secondary outcome, showed significant improvement in dyspnea with glycopyrronium/indacaterol vs. tiotropium but not with glycopyrronium/indacaterol vs. either monotherapy.(49) Umeclidinium/vilanterol, in a 24-week study in which the degree of dyspnea was a secondary outcome, was shown to be more likely to achieve a decrease in dyspnea, as measured by the TDI, when compared with vilanterol alone but not when compared with umeclidinium alone.(43) In two randomized, parallel studies involving a total of more than 3,000 patients, a higher proportion of patients reached the MCID of the TDI with aclidinium/formoterol than with either monotherapy.(45)
Data from a meta-analysis of the efficacy and safety of LABA/LAMA combinations vs. LABAs or LAMAs alone in the treatment of patients with moderate-to-severe COPD, using data from 23 randomized clinical trials of at least 12 weeks' duration, showed that patients on LABA/LAMA achieved better TDI scores than did those on monotherapy and that LABA/LAMA combinations were more effective in reducing the number of (moderate-to-severe) ECOPD when compared with LABAs but not when compared with LAMAs.(50) The evidence indicates that, in terms of efficacy, LABA/LAMA combinations provide more benefits than do LABA and LAMA monotherapies in patients with moderate-to-very-severe COPD who remain symptomatic, because of the improvement in TDI scores. The effect of LABA/LAMA combinations in preventing ECOPD appears to be greater than that of LABAs alone, but it has not yet been conclusively demonstrated to be greater than that of LAMAs alone.
6. WHICH PATIENTS WITH COPD BENEFIT MOST FROM LABA/ICS COMBINATIONS? ICSs modify gene transcription in the cell nucleus, increasing the production of anti-inflammatory proteins and the amount of β2 receptors on the cell surface, which explains the synergistic action of ICSs when combined with LABAs. In contrast, corticosteroid resistance and poor corticosteroid response have been reported in patients with COPD.(51)
ICSs can cause several side effects: candidiasis; dysphonia; superficial hematomas secondary to minor trauma; osteopenia; cataracts; glaucoma; diabetes mellitus; adrenal suppression; mycobacterial infections (including tuberculosis); and pneumonia. Pneumonia has been the subject of several publications and is associated with long-term use of ICSs, high doses, and more potent corticosteroids, as well as with smokers, previous episodes of ECOPD or pneumonia, age > 55 years, body mass index < 25 kg/m2, and severe airway obstruction.(52)
The use of ICSs in combination with LABAs has been mentioned as a therapeutic option aimed at reducing the number of ECOPD and improving quality of life and pulmonary function. Meta-analyses have confirmed that LABA/ICS combinations, as compared with LABAs or ICSs alone, are superior in terms of improvement in pulmonary function, although one may question the mean difference not reaching the current MCID for these outcomes. In terms of improvement in quality of life, LABA/ICS combinations appear to be superior to either monotherapy in patients with COPD and an FEV1 < 50% of predicted.(53)
Blood eosinophil levels may be a predictor of ICS response in individuals with COPD. One study showed that patients with COPD and pretreatment blood eosinophil levels ≥ 2% had a greater reduction in the frequency of ECOPD with LABA/ICS combination therapy than did those with pretreatment blood eosinophil levels < 2%.(54) LABA/ICS combination therapy is also indicated when both COPD and asthma are present.(55)
Patients on LABA/ICS should be carefully evaluated if ICS discontinuation is planned. The ICS can be discontinued in all non-exacerbators who were started on it although there was no indication for it. ICS discontinuation is possibly associated with an increase in the rate of ECOPD per year, worsening of symptoms, and worsening of pulmonary function. This effect is more pronounced in patients with peripheral eosinophilia.(56-58)
Although COPD is an inflammatory disease, the accumulation of evidence regarding the side effects of ICSs and the uncertainties about the action of ICSs in patients with COPD result in the LABA/ICS option being indicated to treat patients with COPD and asthma, patients who have ECOPD and have had an unsatisfactory response to LABA/LAMA, and those with the COPD exacerbator phenotype and peripheral eosinophilia. Eosinophil cut-off values indicating benefit of ICS therapy remain controversial and require confirmation in future studies.
7. IN WHICH CLINICAL CONDITION SHOULD A LAMA BE ADDED TO LABA/ICS COMBINATION THERAPY (TRIPLE THERAPY)? The addition of a LAMA to LABA/ICS combination therapy for the treatment of obstructive diseases is called triple therapy. Treating COPD systematically requires individualized clinical judgment in searching for appropriate treatment options. Although LABA/ICS/LAMA triple therapy is routinely used in clinical practice, there are important issues regarding this treatment modality that need to be clarified.
Studies involving patients with severe or very severe COPD who had more than one ECOPD per year have reported a reduction in the number of hospitalizations and ECOPD with LABA/ICS/LAMA triple therapy. Triple therapy produced improvement in symptoms, pulmonary function, and quality of life scores when compared with LABA/ICS combination therapy and with LAMA monotherapy.(6,59-63) A systematic review comparing triple therapy vs. LABA/ICS combination therapy or tiotropium alone reported improvement in pulmonary function and health-related quality of life for the group treated with triple therapy. However, no differences were observed in the number of ECOPD or in the occurrence of pneumonia, dyspnea, or severe adverse events. The safety profile of triple therapy was similar to that of other treatment options available.(64,65) Observational studies have demonstrated that a prescribing preference for triple therapy exists in several regions of the world, despite the lack of clear criteria for its use, as recommended in guidelines.(66)
The heterogeneity of COPD allows the identification of subgroups of patients with distinct clinical features for whom triple therapy can be indicated. On the basis of the above data, we recommend that LABA/ICS/LAMA triple therapy be used in patients with COPD who remain symptomatic despite LABA/LAMA combination therapy, in those who have ECOPD (2 or more per year) despite maximal bronchodilator therapy with LABA/LAMA, and in patients with COPD and asthma who remain symptomatic despite LABA/ICS combination therapy.(67)
Post hoc analyses from clinical trials suggest that increased serum eosinophil levels can be a biomarker for future risk of ECOPD in exacerbators, as well as predicting the benefits of ICS therapy in preventing ECOPD.(54,58,68,69) The finding of an eosinophil count greater than 300 cells/µL in patients with moderate-to-severe COPD, with a history of ECOPD, and receiving LABA/LAMA can aid in making a decision to initiate triple therapy.(54,70) However, future prospective clinical trials are needed to validate the use of eosinophil counts and to determine a cut-off point for them so that they can be useful in daily practice.(71,72)
8. WHAT IS THE INDICATION FOR ADDING ROFLUMILAST TO PREVENT ECOPD?
Roflumilast is a selective phosphodiesterase-4 (PDE4) inhibitor and acts by blocking this enzyme activity, increasing intracellular levels of cAMP, which results in reduction of cellular inflammatory activity. PDE4 receptors are also expressed in the airway smooth muscle cells; however, this direct bronchodilator effect is modest.(73,74)
Roflumilast is indicated for the treatment of patients with severe or very severe COPD (FEV1 < 50% of predicted) who continue to have ECOPD, cough, and phlegm despite maximal inhaled therapy. The recommended dose is 500 µg/day orally, and the long half-life of the terminal N-oxide metabolite of roflumilast allows the drug to be administered in a single daily dose.(75)
A post hoc evaluation of the initial studies of roflumilast involving a total of 2,686 patients showed a significant reduction of 14.3% in ECOPD in patients with COPD receiving the recommended dose of 500 µg/day vs. placebo over 52 weeks of evaluation. The factors associated with this reduction were presence of chronic bronchitis (reduction of 26.2%); cough (reduction of 20.9%); expectoration (reduction of 17.8%); and concomitant ICS use (reduction of 18.8%).(76)
A recent study conducted in 380 centers in 17 countries and involving 2,354 randomized patients (1,178 receiving roflumilast and 1,176 receiving placebo) showed that the rate of moderate or severe ECOPD was reduced with roflumilast vs. placebo (28.5%), but this difference did not reach significance. The proportion of patients who did not have severe ECOPD over the 52 weeks of treatment was greater in the roflumilast group than in the placebo group (54.2% vs. 48.5%). The time to the onset of severe ECOPD was 319 and 286 days, respectively, in the roflumilast and placebo groups, with the difference not being significant.(77)
A meta-analysis of 14 studies involving 12,654 patients with severe or very severe COPD associated with chronic bronchitis showed that roflumilast in combination with an ICS, a LABA, and a LAMA significantly improves FEV1 (mean, 45.60 mL) and reduces the frequency of moderate and severe ECOPD compared with placebo (OR = 0.77).(78) In a post hoc analysis of the same study, in patients with more than three ECOPD per year, the rate of moderate or severe ECOPD decreased by 39% in the group receiving roflumilast compared with the group receiving placebo, with the difference being significant.(79)
Roflumilast is generally well tolerated with adverse events consistent with those expected for PDE4 inhibitors. However, it has more adverse effects than do the inhaled drugs used in the treatment of COPD. The most common adverse effects, reported in combined data from clinical trials involving 8,630 patients, are gastrointestinal disorders (diarrhea and nausea), decreased appetite, insomnia, depression, headache, and weight loss. These adverse effects are stronger at the beginning of treatment, are reversible, and improve over time (generally within 4 weeks).(79) In another combined safety analysis, which included data from 14 clinical trials of roflumilast in 12,054 patients, the rates of adverse events in the roflumilast and placebo groups were, respectively, 67.2% and 62.8%, whereas the rates of severe adverse events were 13.5% vs. 14.2%.(77)
The evidence from those studies provides additional information on the patient subgroup that is likely to benefit from the addition of roflumilast to the treatment regimen. Roflumilast is indicated for patients with severe or very severe COPD (FEV1 < 50% of predicted), chronic bronchitis (cough and expectoration), and frequent ECOPD despite appropriate inhaled therapy.
9. DOES THE PROPHYLACTIC USE OF ANTIBIOTICS IN PATIENTS WITH STABLE COPD PREVENT ECOPD? ECOPD are triggered by viral infections or by acquisition of a new bacterial strain in the lower airways. Studies suggest that the presence of bacteria in the lower airways contributes to chronic inflammation, resulting in disease progression. Therefore, it is possible that, in chronically infected patients, the bacterial load reduction caused by long-term use of antibiotics reduces the frequency and severity of ECOPD. Macrolides have been indicated because of their anti-inflammatory and immunomodulatory effects. In addition, macrolides alter biofilm production and improve phagocytosis and bacterial clearance by alveolar macrophages.(80-82)
A study on the use of erythromycin for 12 months found that such use led to a reduction in ECOPD and in the risk of hospitalization.(83) In a subsequent study, it was demonstrated that the duration of ECOPD was shorter with continued use of erythromycin.(84) In 2011, a study evaluating 1,142 patients on long-term home oxygen therapy or with a history of ECOPD found that, when added to the usual treatment, daily azithromycin for 1 year reduced the frequency of ECOPD and improved quality of life.(85)
A meta-analysis of six studies reported a 37% reduction in the risk of ECOPD with antibiotic therapy compared with placebo.(86) .A systematic review of seven studies involving more than 3,000 patients identified a significant effect of continued antibiotic therapy on the reduction in the number of ECOPD.(87)
The use of intermittent courses of oral fluoroquinolone therapy reduced the likelihood of ECOPD by approximately 25%, as demonstrated in a study evaluating treatment with daily moxifloxacin for 5 days every 8 weeks for a total of 6 courses.(88) Patients with mucopurulent sputum before treatment experienced a reduction of up to 45% in ECOPD. However, the lack of studies, the risk of inducing bacterial resistance, and the side effects of chronic antibiotic use limit the routine use of this strategy.(88)
The use of inhaled antibiotic therapy in patients with COPD cannot be recommended yet because of the lack of randomized clinical trials in which the efficacy of such use has been proven. Despite the reduction in bronchial inflammation in patients chronically colonized with Pseudomonas aeruginosa after 2 weeks of treatment with inhaled tobramycin, the few existing studies have been unable to demonstrate clinical benefits of inhaled antibiotic therapy in preventing ECOPD.(89,90)
The indication for prophylactic antibiotics in COPD should be determined on a case-by-case basis. Prophylactic antibiotics are a third-line therapy for the treatment of exacerbators. The available evidence lends support to the use of azithromycin 250 mg daily or azithromycin 500 mg three times a week or the use of erythromycin 500 mg twice daily for 1 year in patients with severe or very severe COPD and in exacerbators despite usual pharmacological treatment. Long-term use is associated with an increased risk of adverse events and development of bacterial resistance. Special care should be taken in patients with concomitant heart disease, tachycardia at rest, or a history of arrhythmias. Ototoxicity and gastrointestinal side effects should also be monitored. It is recommended that, before initiation of such therapy, sputum samples be collected for bacterial and mycobacterial culture, given that continued use of a macrolide can make it difficult to diagnose chronic lung infections with low-virulence microorganisms.(91,92)
10. CAN N-ACETYLCYSTEINE (NAC) BE USED FOR PREVENTING ECOPD?There are consistent data in the literature showing that airway oxidative stress in patients with COPD plays an important role in the development of the disease and is associated with future risk of ECOPD and with a greater influx of inflammatory cells and inflammatory cytokines. The use of antioxidant and anti-inflammatory agents in COPD has been studied for the control of ECOPD. In this context, the efficacy and safely of NAC in COPD are being investigated regarding prevention of ECOPD.(93)
NAC has direct action, because of the presence of the free sulfhydryl group, which serves as a ready source of redox equivalents, and indirect action, because of the intracellular replacement of glutathione antioxidant levels. However, there is still much discussion regarding the efficacy of NAC in controlling ECOPD events and regarding the optimal dose for controlling such events.(94)
In a randomized clinical trial conducted in the United States,(95) 51 patients with COPD due to tobacco exposure and with symptoms of chronic bronchitis (cough and secretion) were allocated to receive NAC, 1,800 mg twice daily, or placebo for 8 weeks. However, the sample size did not reach the goal of 130 patients, which may have influenced the results showing no change in quality of life, in pulmonary function, or in markers of systemic inflammation and oxidative stress. The most common adverse events were mild nausea and diarrhea.(95) In contrast, a randomized study conducted in China, comparing NAC, 600 mg twice daily, vs. placebo in 1,006 patients with COPD and at least two ECOPD in the preceding 2 years, showed that NAC treatment was more effective in patients with moderate COPD than in those with severe COPD, with a significant reduction in the rate of ECOPD after 1 year. The time to first ECOPD was not different between the groups. Ten percent of the patients in the NAC group and 9% of those in the placebo group had serious adverse events, most of which were due to hospitalization for ECOPD.(96) Another randomized study conducted in China, comparing NAC, 600 mg twice daily, for 1 year vs. placebo in 120 patients, demonstrated a significant reduction in the rate of ECOPD in the NAC group compared with the control group (0.96 vs. 1.71 ECOPD/patient/year).(97) In 2005, a study comparing NAC, 600 mg once daily, for 3 years vs. placebo in 523 patients showed that there was no difference between the NAC and the control groups. However, in the subgroup of patients who were not receiving ICSs (155 patients), there was a 26% reduction in the risk of ECOPD.(98)
Two meta-analyses showed that NAC treatment reduced the rate of ECOPD (risk ratio = 0.85; 95% CI: 0.76-0.96). The findings were consistent regarding the reduction in the number of exacerbations with treatment with high doses (1,200 mg) of NAC in patients with COPD and with treatment with low doses (600 mg) of NAC in patients with chronic bronchitis who did not have COPD, but NAC had no effect on pulmonary function. Therefore, the recent studies show that NAC can be safely used for the prevention of ECOPD when used for more than 6 months and at daily doses greater than 1,200 mg.(99,100)
Given the safety profile of NAC and the evidence of its efficacy, its use as a third-line drug in the prevention of ECOPD is recommended; the profile of patients who obtain greater benefits from NAC treatment appears to be that of patients with chronic bronchitis, but this is still controversial.
REFERENCES1. Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356(8):775-89 https://doi.org/10.1056/NEJMoa063070
2. Menezes AM, Macedo SE, Noal RB, Fiterman J, Cukier A, Chatkin JM, et al. Pharmacological treatment of COPD. J Bras Pneumol. 2011;37(4):527-43 https://doi.org/10.1590/S1806-37132011000400016
3. Reichert J, Araújo AJ, Gonçalves CM, Godoy I, Chatkin JM, Sales MP, et al. Diretrizes para cessação do tabagismo da SBPT: 2008. J Bras Pneumol. 2008;34(10):845-80 https://doi.org/10.1590/S1806-37132008001000014
4. Global Initiative for Chronic Obstructive Lung Disease [homepage on the Internet. Bethesda: GOLD [cited 2017 Dec 10]. Global Strategy for the Diagnosis, Management and Prevention of COPD 2016. Available from: http://www.goldcopd.org/
5. Agusti A, Calverley PM, Celli B, Coxson HO, Edwards LD, Lomas DA, et al. Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respir Res. 2010;11:122 https://doi.org/10.1186/1465-9921-11-122
6. Miravitlles M, Worth H, Soler Cataluna JJ, Price D, De Benedetto F, Roche N, et al. Observational study to characterise 24-hour COPD symptoms and their relationship with patient-reported outcomes: results from the ASSESS study. Respir Res. 2014;15:122 https://doi.org/10.1186/s12931-014-0122-1
7. Nishimura K, Izumi T, Tsukino M, Oga T. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest. 2002;121(5):1434-40 https://doi.org/10.1378/chest.121.5.1434
8. van Buul AR, Kasteleyn MJ, Chavannes NH, Taube C. Morning symptoms in COPD: a treatable yet often overlooked factor. Expert Rev Respir Med. 2017;11(4):311-22 https://doi.org/10.1080/17476348.2017.1305894
9. Silva GP, Morano MT, Viana CM, Magalhaes CB, Pereira ED. Portuguese-language version of the COPD Assessment Test: validation for use in Brazil. J Bras Pneumol. 2013;39(4):402-8 https://doi.org/10.1590/S1806-37132013000400002
10. Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD Assessment Test. Eur Resp J. 2009;34(3):648-54 https://doi.org/10.1183/09031936.00102509
11. Ghobadi H, Ahari SS, Kameli A, Lari SM. The Relationship between COPD Assessment Test (CAT) Scores and Severity of Airflow Obstruction in Stable COPD Patients. Tanaffos. 2012;11(2):22-6
12. Kim S, Oh J, Kim YI, Ban HJ, Kwon YS, Oh IJ, et al. Differences in classification of COPD group using COPD assessment test (CAT) or modified Medical Research Council (mMRC) dyspnea scores: a cross-sectional analyses. BMC Pulm Med. 2013;13:35 https://doi.org/10.1186/1471-2466-13-35
13. Hodgkin JE. Prognosis in chronic obstructive pulmonary disease. Clin Chest Med. 1990;11(3):555-69
14. Antonelli Incalzi R, Fuso L, De Rosa M, Forastiere F, Rapiti E, Nardecchia B, et al. Co-morbidity contributes to predict mortality of patients with chronic obstructive pulmonary disease. Eur Resp J. 1997;10(12):2794-800 https://doi.org/10.1183/09031936.97.10122794
15. Domingo-Salvany A, Lamarca R, Ferrer M, Garcia-Aymerich J, Alonso J, Félez M, et al. Health-related quality of life and mortality in male patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2002;166(5):680-5 https://doi.org/10.1164/rccm.2112043
16. Schols AM, Slangen J, Volovics L, Wouters EF. Weight loss is a reversible factor in the prognosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157(6 Pt 1):1791-7 https://doi.org/10.1164/ajrccm.157.6.9705017
17. Groenewegen KH, Schols AM, Wouters EF. Mortality and mortality-related factors after hospitalization for acute exacerbation of COPD. Chest. 2003;124(2):459-67 https://doi.org/10.1378/chest.124.2.459
18. Almagro P, Calbo E, Ochoa de Echagüen A, Barreiro B, Quintana S, Heredia JL, et al. Mortality after hospitalization for COPD. Chest. 2002;121(5):1441-8 https://doi.org/10.1378/chest.121.5.1441
19. Celli BR, Cote CG, Lareau SC, Meek PM. Predictors of Survival in COPD: more than just the FEV1. Resp Med. 2008;102 Suppl 1:S27-35 https://doi.org/10.1016/S0954-6111(08)70005-2
20. Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GK, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106(2):196-204 https://doi.org/10.7326/0003-4819-106-2-196
21. Rodriguez-Roisin R. Toward a consensus definition for COPD exacerbations. Chest. 2000;117(5 Suppl 2):398S-401S https://doi.org/10.1378/chest.117.5_suppl_2.398S
22. Wedzicha JA, Brill SE, Allinson JP, Donaldson GC. Mechanisms and impact of the frequent exacerbator phenotype in chronic obstructive pulmonary disease. BMC Med. 2013;11:181 https://doi.org/10.1186/1741-7015-11-181
23. McAllister DA, Maclay JD, Mills NL, Leitch A, Reid P, Carruthers R, et al. Diagnosis of myocardial infarction following hospitalisation for exacerbation of COPD. Eur Resp J. 2012;39(5):1097-103 https://doi.org/10.1183/09031936.00124811
24. Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60(11):925-31 https://doi.org/10.1136/thx.2005.040527
25. Anzueto A. Impact of exacerbations on COPD. Eur Resp Rev. 2010;19(116):113-8 https://doi.org/10.1183/09059180.00002610
26. Hurst JR, Vestbo J, Anzueto A, Locantore N, Müllerova H, Tal-Singer R, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128-38 https://doi.org/10.1056/NEJMoa0909883
27. Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002;57(10):847-52 https://doi.org/10.1136/thorax.57.10.847
28. Halpin DM, Decramer M, Celli B, Kesten S, Liu D, Tashkin DP. Exacerbation frequency and course of COPD. Int J Chron Obstruct Pulmon Dis. 2012;7:653-61 https://doi.org/10.2147/COPD.S34186
29. Miravitlles M, Ferrer M, Pont A, Zalacain R, Alvarez-Sala JL, Masa F, et al. Effect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow up study. Thorax. 2004;59(5):387-95 https://doi.org/10.1136/thx.2003.008730
30. Spencer S, Calverley PM, Burge PS, Jones PW. Impact of preventing exacerbations on deterioration of health status in COPD. Eur Resp J. 2004;23(5):698-702 https://doi.org/10.1183/09031936.04.00121404
31. Appleton S, Poole P, Smith B, Veale A, Lasserson TJ, Chan MM. Long-acting beta2-agonists for poorly reversible chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2006;(3):CD001104 https://doi.org/10.1002/14651858.cd001104.pub2
32. Barr RG, Bourbeau J, Camargo CA, Ram FS. Inhaled tiotropium for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2005(2):CD002876
33. Barnes PJ. Asthma-COPD Overlap. Chest. 2016;149(1):7-8 https://doi.org/10.1016/j.chest.2015.08.017
34. Decramer ML, Chapman KR, Dahl R, Frith P, Devouassoux G, Fritscher C, et al. Once-daily indacaterol versus tiotropium for patients with severe chronic obstructive pulmonary disease (INVIGORATE): a randomised, blinded, parallel-group study. Lancet Respir Med. 2013;1(7):524-33 https://doi.org/10.1016/S2213-2600(13)70158-9
35. O'Donnell DE, Neder JA, Elbehairy AF. Physiological impairment in mild COPD. Respirology. 2016;21(2):211-23 https://doi.org/10.1111/resp.12619
36. Enright P. HRCT-defined emphysema is not COPD to be treated with inhalers. Thorax. 2014;69(5):401-2 https://doi.org/10.1136/thoraxjnl-2013-203497
37. Bridevaux PO, Gerbase MW, Probst-Hensch NM, Schindler C, Gaspoz JM, Rochat T. Long-term decline in lung function, utilisation of care and quality of life in modified GOLD stage 1 COPD. Thorax. 2008;63(9):768-74 https://doi.org/10.1136/thx.2007.093724
38. Vestbo J, Sørensen T, Lange P, Brix A, Torre P, Viskum K. Long-term effect of inhaled budesonide in mild and moderate chronic obstructive pulmonary disease: a randomised controlled trial. Lancet. 1999;353(9167):1819-23 https://doi.org/10.1016/S0140-6736(98)10019-3
39. Casaburi R, Maltais F, Porszasz J, Albers F, Deng Q, Iqbal A, et al. Effects of tiotropium on hyperinflation and treadmill exercise tolerance in mild to moderate chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2014;11(9):1351-61 https://doi.org/10.1513/AnnalsATS.201404-174OC
40. Johansson G, Lindberg A, Romberg K, Nordstrom L, Gerken F, Roquet A. Bronchodilator efficacy of tiotropium in patients with mild to moderate COPD. Prim Care Respir J. 2008;17(3):169-75 https://doi.org/10.3132/pcrj.2008.00037
41. Fernandes FL, Pavezi VA, Dias SA Jr, Pinto RM, Stelmach R, Cukier A. Short-term effect of tiotropium in COPD patients being treated with a beta2 agonist. J Bras Pneumol. 2010;36(2):181-9 https://doi.org/10.1590/S1806-37132010000200005
42. Wedzicha JA, Decramer M, Ficker JH, Niewoehner DE, Sandstrom T, Taylor AF, et al. Analysis of chronic obstructive pulmonary disease exacerbations with the dual bronchodilator QVA149 compared with glycopyrronium and tiotropium (SPARK): a randomised, double-blind, parallel-group study. Lancet Resp Med. 2013;1(3):199-209 https://doi.org/10.1016/S2213-2600(13)70052-3
43. Decramer M, Anzueto A, Kerwin E, Kaelin T, Richard N, Crater G, et al. Efficacy and safety of umeclidinium plus vilanterol versus tiotropium, vilanterol, or umeclidinium monotherapies over 24 weeks in patients with chronic obstructive pulmonary disease: results from two multicentre, blinded, randomised controlled trials. Lancet Resp Med. 2014;2(6):472-86 https://doi.org/10.1016/S2213-2600(14)70065-7
44. Donohue JF, Niewoehner D, Brooks J, O'Dell D, Church A. Safety and tolerability of once-daily umeclidinium/vilanterol 125/25 mcg and umeclidinium 125 mcg in patients with chronic obstructive pulmonary disease: results from a 52-week, randomized, double-blind, placebo-controlled study. Resp Res. 2014;15:78
45. Bateman ED, Chapman KR, Singh D, D'Urzo AD, Molins E, Leselbaum A, et al. Aclidinium bromide and formoterol fumarate as a fixed-dose combination in COPD: pooled analysis of symptoms and exacerbations from two six-month, multicentre, randomised studies (ACLIFORM and AUGMENT). Resp Res. 2015;16:92 https://doi.org/10.1186/s12931-015-0250-2
46. Miravitlles M, Chapman KR, Chuecos F, Ribera A, Gil EG. The efficacy of aclidinium/formoterol on lung function and symptoms in patients with COPD categorized by symptom status: a pooled analysis. Int J Chron Obstruct Pulmon Dis 2016;11:2041-53 https://doi.org/10.2147/COPD.S114566
47. Derom E, Brusselle GG, Joos GF. Efficacy of tiotropium-olodaterol fixed-dose combination in COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:3163-77 https://doi.org/10.2147/COPD.S92840
48. Mahler DA, Decramer M, D'Urzo A, Worth H, White T, Alagappan VK, et al. Dual bronchodilation with QVA149 reduces patient-reported dyspnoea in COPD: the BLAZE study. European Resp J. 2014;43(6):1599-609 https://doi.org/10.1183/09031936.00124013
49. Bateman ED, Ferguson GT, Barnes N, Gallagher N, Green Y, Henley M, et al. Dual bronchodilation with QVA149 versus single bronchodilator therapy: the SHINE study. European Resp J. 2013;42(6):1484-94 https://doi.org/10.1183/09031936.00200212
50. Oba Y, Sarva ST, Dias S. Efficacy and safety of long-acting β-agonist/long-acting muscarinic antagonist combinations in COPD: a network meta-analysis. Thorax. 2016;71(1):15-25 https://doi.org/10.1136/thoraxjnl-2014-206732
51. Keatings VM, Jatakanon A, Worsdell YM, Barnes PJ. Effects of inhaled and oral glucocorticoids on inflammatory indices in asthma and COPD. Am J Respir Crit Care Med. 1997;155(2):542-8 https://doi.org/10.1164/ajrccm.155.2.9032192
52. Crim C, Dransfield MT, Bourbeau J, Jones PW, Hanania NA, Mahler DA, et al. Pneumonia risk with inhaled fluticasone furoate and vilanterol compared with vilanterol alone in patients with COPD. Ann Am Thorac Soc. 2015;12(1):27-34 https://doi.org/10.1513/AnnalsATS.201409-413OC
53. Nannini LJ, Poole P, Milan SJ, Kesterton A. Combined corticosteroid and long-acting beta(2)-agonist in one inhaler versus inhaled corticosteroids alone for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2013(8):CD006826
54. Pavord ID, Lettis S, Locantore N, Pascoe S, Jones PW, Wedzicha JA, et al. Blood eosinophils and inhaled corticosteroid/long-acting β-2 agonist efficacy in COPD. Thorax. 2016;71(2):118-25 https://doi.org/10.1136/thoraxjnl-2015-207021
55. Silva GE, Sherrill DL, Guerra S, Barbee RA. Asthma as a risk factor for COPD in a longitudinal study. Chest. 2004;126(1):59-65 https://doi.org/10.1378/chest.126.1.59
56. Wouters EF, Postma DS, Fokkens B, Hop WC, Prins J, Kuipers AF, et al. Withdrawal of fluticasone propionate from combined salmeterol/fluticasone treatment in patients with COPD causes immediate and sustained disease deterioration: a randomised controlled trial. Thorax. 2005;60(6):480-7 https://doi.org/10.1136/thx.2004.034280
57. Magnussen H, Disse B, Rodriguez-Roisin R, Kirsten A, Watz H, Tetzlaff K, et al. Withdrawal of inhaled glucocorticoids and exacerbations of COPD. N Engl J Med. 2014;371(14):1285-94 https://doi.org/10.1056/NEJMoa1407154
58. Watz H, Tetzlaff K, Wouters EF, Kirsten A, Magnussen H, Rodriguez-Roisin R, et al. Blood eosinophil count and exacerbations in severe chronic obstructive pulmonary disease after withdrawal of inhaled corticosteroids: a post-hoc analysis of the WISDOM trial. Lancet Respir Med. 2016;4(5):390-8 https://doi.org/10.1016/S2213-2600(16)00100-4
59. Aaron SD, Vandemheen KL, Fergusson D, Maltais F, Bourbeau J, Goldstein R, et al. Tiotropium in combination with placebo, salmeterol, or fluticasone-salmeterol for treatment of chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med. 2007;146(8):545-55 https://doi.org/10.7326/0003-4819-146-8-200704170-00152
60. Welte T, Miravitlles M, Hernandez P, Eriksson G, Peterson S, Polanowski T, et al. Efficacy and tolerability of budesonide/formoterol added to tiotropium in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2009;180(8):741-50 https://doi.org/10.1164/rccm.200904-0492OC
61. Short PM, Williamson PA, Elder DHJ, Lipworth SIW, Schembri S, Lipworth BJ. The impact of tiotropium on mortality and exacerbations when added to inhaled corticosteroids and long-acting β-agonist therapy in COPD. Chest. 2012;141(1):81-6 https://doi.org/10.1378/chest.11-0038
62. Singh D, Brooks J, Hagan G, Cahn A, O'Connor BJ. Superiority of "triple" therapy with salmeterol/fluticasone propionate and tiotropium bromide versus individual components in moderate to severe COPD. Thorax. 2008;63(7):592-8 https://doi.org/10.1136/thx.2007.087213
63. Jung KS, Park HY, Park SY, Kim SK, Kim YK, Shim JJ, et al. Comparison of tiotropium plus fluticasone propionate/salmeterol with tiotropium in COPD: a randomized controlled study. Respir Med. 2012;106(3):382-9 https://doi.org/10.1016/j.rmed.2011.09.004
64. Rodrigo GJ, Plaza V, Castro-Rodríguez JA. Comparison of three combined pharmacological approaches with tiotropium monotherapy in stable moderate to severe COPD: a systematic review. Pulm Pharmacol Ther. 2012;25(1):40-7 https://doi.org/10.1016/j.pupt.2011.10.006
65. Singh D, Papi A, Corradi M, Pavlisova I, Montagna I, Francisco C, et al. Single inhaler triple therapy versus inhaled corticosteroid plus long-acting β2-agonist therapy for chronic obstructive pulmonary disease (TRILOGY): a double-blind, parallel group, randomised controlled trial. Lancet. 2016;388(10048):963-73 https://doi.org/10.1016/S0140-6736(16)31354-X
66. Brusselle G, Price D, Gruffydd-Jones K, Miravitlles M, Keininger DL, Stewart R, et al. The inevitable drift to triple therapy in COPD: an analysis of prescribing pathways in the UK. Int J Chron Obstruct Pulmon Dis. 2015;10:2207-17
67. Andreeva-Gateva PA, Stamenova E, Gatev T. The place of inhaled corticosteroids in the treatment of chronic obstructive pulmonary disease: a narrative review. Postgrad Med. 2016;128(5):474-84 https://doi.org/10.1080/00325481.2016.1186487
68. Pascoe S, Locantore N, Dransfield MT, Barnes NC, Pavord ID. Blood eosinophil counts, exacerbations, and response to the addition of inhaled fluticasone furoate to vilanterol in patients with chronic obstructive pulmonary disease: a secondary analysis of data from two parallel randomised controlled trials. Lancet Respir Med. 2015;3(6):435-42 https://doi.org/10.1016/S2213-2600(15)00106-X
69. Siddiqui SH, Guasconi A, Vestbo J, Jones P, Agusti A, Paggiaro P, et al. Blood Eosinophils: A Biomarker of Response to Extrafine Beclomethasone/Formoterol in Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2015;192(4):523-5 https://doi.org/10.1164/rccm.201502-0235LE
70. Wedzicha JA, Banerji D, Chapman KR, Vestbo J, Roche N, Ayers RT, et al. Indacaterol-Glycopyrronium versus Salmeterol-Fluticasone for COPD. N Engl J Med. 2016;374(23):2222-34 https://doi.org/10.1056/NEJMoa1516385
71. Vogelmeier CF, Criner GJ, Martínez FJ, Anzueto A, Barnes PJ, Bourbeau J, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report: GOLD Executive Summary. The Eur Respir J. 2017 49(3). pii: 1700214 https://doi.org/10.1183/13993003.00214-2017
72. Montuschi P, Malerba M, Macis G, Mores N, Santini G. Triple inhaled therapy for chronic obstructive pulmonary disease. Drug Discov Today. 2016;21(11):1820-7 https://doi.org/10.1016/j.drudis.2016.07.009
73. Vignola AM. PDE4 inhibitors in COPD--a more selective approach to treatment. Respir Med. 2004;98(6):495-503 https://doi.org/10.1016/j.rmed.2003.12.012
74. Taegtmeyer AB, Leuppi JD, Kullak-Ublick GA. Roflumilast--a phosphodiesterase-4 inhibitor licensed for add-on therapy in severe COPD. Swiss Med Wkly. 2012;142:w13628 https://doi.org/10.4414/smw.2012.13628
75. Rabe KF, Bateman ED, O'Donnell D, Witte S, Bredenbröker D, Bethke TD. Roflumilast--an oral anti-inflammatory treatment for chronic obstructive pulmonary disease: a randomised controlled trial. Lancet. 2005;366(9485):563-71 https://doi.org/10.1016/S0140-6736(05)67100-0
76. Calverley PM, Rabe KF, Goehring UM, Kristiansen S, Fabbri LM, Martinez FJ, et al. Roflumilast in symptomatic chronic obstructive pulmonary disease: two randomised clinical trials. Lancet. 2009;374(9691):685-94 https://doi.org/10.1016/S0140-6736(09)61255-1
77. Martinez FJ, Rabe KF, Sethi S, Pizzichini E, McIvor A, Anzueto A, et al. Effect of Roflumilast and Inhaled Corticosteroid/Long-Acting β2-Agonist on Chronic Obstructive Pulmonary Disease Exacerbations (RE(2)SPOND). A Randomized Clinical Trial. Am J Respir Crit Care Med. 2016;194(5):559-67 https://doi.org/10.1164/rccm.201607-1349OC
78. Chong J, Leung B, Poole P. Phosphodiesterase 4 inhibitors for chronic obstructive pulmonary disease. The Cochrane Database Syst Rev. 2013;(11):CD002309 https://doi.org/10.1002/14651858.cd002309.pub4
79. Wedzicha JA, Calverley PM, Rabe KF. Roflumilast: a review of its use in the treatment of COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:81-90 https://doi.org/10.2147/COPD.S89849
80. Maraffi T, Piffer F, Cosentini R. Prophylactic antibiotic therapy in chronic obstructive pulmonary disease. Ther Adv Respir Dis. 2010;4(3):135-42 https://doi.org/10.1177/1753465810368552
81. Wilson R, Sethi S, Anzueto A, Miravitlles M. Antibiotics for treatment and prevention of exacerbations of chronic obstructive pulmonary disease. J Infect. 2013;67(6):497-515 https://doi.org/10.1016/j.jinf.2013.08.010
82. Yamaya M, Azuma A, Takizawa H, Kadota J, Tamaoki J, Kudoh S. Macrolide effects on the prevention of COPD exacerbations. Eur Respir J. 2012;40(2):485-94 https://doi.org/10.1183/09031936.00208011
83. Suzuki T, Yanai M, Yamaya M, Satoh-Nakagawa T, Sekizawa K, Ishida S, et al. Erythromycin and common cold in COPD. Chest. 2001;120(3):730-3 https://doi.org/10.1378/chest.120.3.730
84. Seemungal TA, Wilkinson TM, Hurst JR, Perera WR, Sapsford RJ, Wedzicha JA. Long-term erythromycin therapy is associated with decreased chronic obstructive pulmonary disease exacerbations. Am J Respir Crit Care Med. 2008;178(11):1139-47 https://doi.org/10.1164/rccm.200801-145OC
85. Albert RK, Connett J, Bailey WC, Casaburi R, Cooper JA Jr, Criner GJ, et al. Azithromycin for prevention of exacerbations of COPD. N Engl J Med. 2011;365(8):689-98. https://doi.org/10.1056/NEJMoa1104623
86. Donath E, Chaudhry A, Hernandez-Aya LF, Lit L. A meta-analysis on the prophylactic use of macrolide antibiotics for the prevention of disease exacerbations in patients with Chronic Obstructive Pulmonary Disease. Respir Med. 2013;107(9):1385-92 https://doi.org/10.1016/j.rmed.2013.05.004
87. Herath SC, Poole P. Prophylactic antibiotic therapy for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev. 2013;(11):CD009764 https://doi.org/10.1002/14651858.cd009764.pub2
88. Sethi S, Jones PW, Theron MS, Miravitlles M, Rubinstein E, Wedzicha JA, et al. Pulsed moxifloxacin for the prevention of exacerbations of chronic obstructive pulmonary disease: a randomized controlled trial. Respir Res. 2010;11:10 https://doi.org/10.1186/1465-9921-11-10
89. Dal Negro R, Micheletto C, Tognella S, Visconti M, Turati C. Tobramycin Nebulizer Solution in severe COPD patients colonized with Pseudomonas aeruginosa: effects on bronchial inflammation. Adv Ther. 2008;25(10):1019-30 https://doi.org/10.1007/s12325-008-0105-2
90. Flume PA, VanDevanter DR, Morgan EE, Dudley MN, Loutit JS, Bell SC, et al. A phase 3, multi-center, multinational, randomized, double-blind, placebo-controlled study to evaluate the efficacy and safety of levofloxacin inhalation solution (APT-1026) in stable cystic fibrosis patients. J Cyst Fibros. 2016;15(4):495-502 https://doi.org/10.1016/j.jcf.2015.12.004
91. Miravitlles M, Anzueto A. Antibiotic prophylaxis in COPD: Why, when, and for whom? Pulm Pharmacol Ther. 2015;32:119-23 https://doi.org/10.1016/j.pupt.2014.05.002
92. Wenzel RP, Fowler AA 3rd, Edmond MB. Antibiotic prevention of acute exacerbations of COPD. N Engl J Med. 2012;367(4):340-7 https://doi.org/10.1056/NEJMct1115170
93. Tse HN, Tseng CZ. Update on the pathological processes, molecular biology, and clinical utility of N-acetylcysteine in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2014;9:825-36 https://doi.org/10.2147/COPD.S51057
94. Sanguinetti CM. N-acetylcysteine in COPD: why, how, and when? Multidiscip Respir Med. 2015;11:8 https://doi.org/10.1186/s40248-016-0039-2
95. Johnson K, McEvoy CE, Naqvi S, Wendt C, Reilkoff RA, Kunisaki KM, et al. High-dose oral N-acetylcysteine fails to improve respiratory health status in patients with chronic obstructive pulmonary disease and chronic bronchitis: a randomized, placebo-controlled trial. Int J Chron Obstruct Pulmon Dis. 2016;11:799-807
96. Zheng JP, Wen FQ, Bai CX, Wan HY, Kang J, Chen P, et al. Twice daily N-acetylcysteine 600 mg for exacerbations of chronic obstructive pulmonary disease (PANTHEON): a randomised, double-blind placebo-controlled trial. Lancet Respir Med. 2014;2(3):187-94 https://doi.org/10.1016/S2213-2600(13)70286-8
97. Tse HN, Raiteri L, Wong KY, Yee KS, Ng LY, Wai KY, et al. High-dose N-acetylcysteine in stable COPD: the 1-year, double-blind, randomized, placebo-controlled HIACE study. Chest. 2013;144(1):106-18 https://doi.org/10.1378/chest.12-2357
98. Decramer M, Rutten-van Molken M, Dekhuijzen PN, Troosters T, van Herwaarden C, Pellegrino R, et al. Effects of N-acetylcysteine on outcomes in chronic obstructive pulmonary disease (Bronchitis Randomized on NAC Cost-Utility Study, BRONCUS): a randomised placebo-controlled trial. Lancet. 2005;365(9470):1552-60 https://doi.org/10.1016/S0140-6736(05)66456-2
99. Fowdar K, Chen H, He Z, Zhang J, Zhong X, Zhang J, et al. The effect of N-acetylcysteine on exacerbations of chronic obstructive pulmonary disease: A meta-analysis and systematic review. Heart Lung. 2017;46(2):120-8 https://doi.org/10.1016/j.hrtlng.2016.12.004
100. Cazzola M, Calzetta L, Page C, Jardim J, Chuchalin AG, Rogliani P, et al. Influence of N-acetylcysteine on chronic bronchitis or COPD exacer-bations: a meta-analysis. Eur Respir Rev. 2015;24(137):451-61 https://doi.org/10.1183/16000617.00002215