TO THE EDITOR:Recently, a letter published in the European Respiratory Review brought attention to a pulmonary infection caused by Cladosporium cladosporioides in an immunocompetent woman.(1) Based on this interesting note, we were able to diagnose a case of alveolar hemorrhage by C. cladosporioides in a previously healthy patient, reinforcing the importance of this fungus in the respiratory tract. To the best of our knowledge, this is the first case of hemorrhagic pneumonia due to C. cladosporioides, and the second report of pulmonary parenchymal infection associated with C. cladosporioides affecting a non-immunocompromised patient, whose main symptom was hemoptysis.
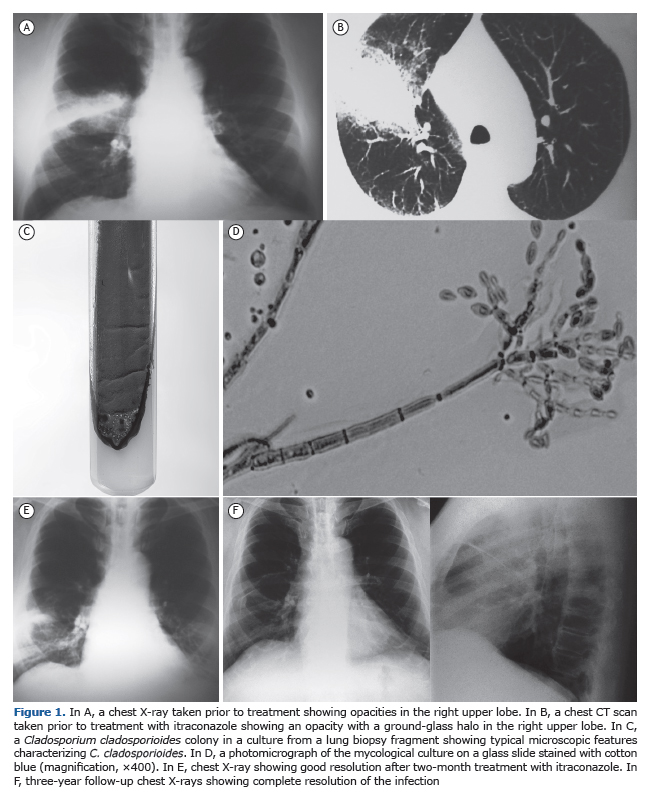
We report the case of a 59-year-old male outpatient who presented with hemoptysis for two weeks. He was an active smoker and had a 25-pack-year smoking history. He had been working in a restaurant in Japan for 5 years and reported having ingested a large number of raw pea-nuts just before the hemoptysis episodes. He came back to Brazil to have this symptom investigated. Clinical examination revealed a good general condition of the patient, no fever or respiratory distress. Auscultation was clear; chest X-ray revealed haziness in the right upper lobe, whereas CT of the chest showed a large opacity with a ground-glass halo in the posterior segment of the upper right lobe (Figures 1A and 1B). Immunological tests were normal, and HIV serology was negative. Fiberoptic bronchoscopy revealed blood in the right upper lobe bronchus; BAL fluid was bloody, and its culture was negative for bacteria and fungi. The patient was started on a seven-day course with amoxicil-lin/clavulanate; no clinical difference was observed. Two weeks later, the patient presented with dyspnea, wheezing, cough, and increased hemoptysis. Surgical lung biopsy was performed and the histopathological examination of the specimen revealed alveolar hemorrhage. Culture from the biopsy fragments was carried out by using ten tubes containing Sabouraud glucose agar without cycloheximide, which were incubated in the darkness at 25ºC and examined daily. Fourteen days later, there was growth of a pure culture presenting as dark green colonies with black reverse. Microculture assays showed conidiophores branching terminally and laterally, allowing the identification of the fungus as C. cladosporioides (Figures 1C and 1D). There was no growth of any type of bacteria in the cultures.
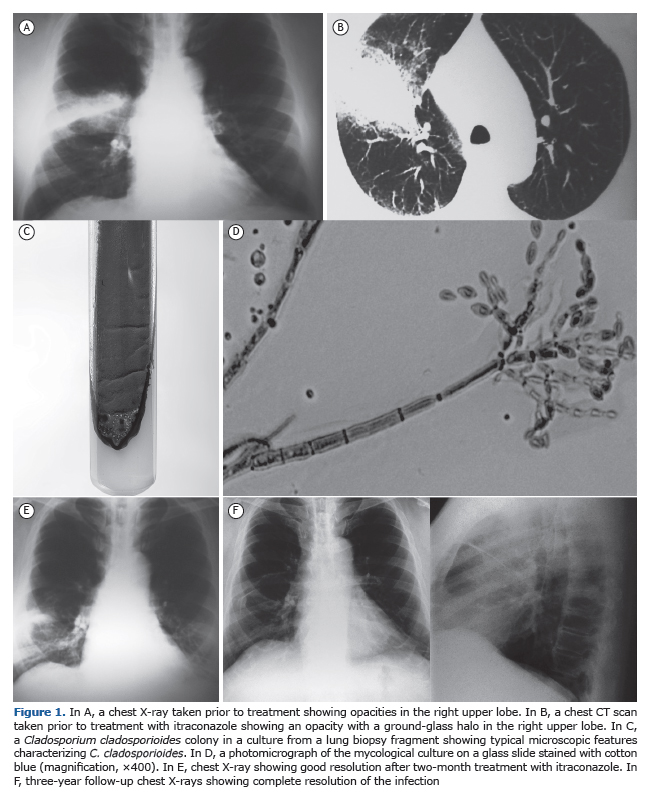
The patient was treated with itraconazole 400 mg daily. Within two months, there was clinical improvement with remission of dyspnea, hemop-tysis, and cough, as well as radiological improvement (Figure 1E). At 3 years of follow-up, chest X-rays revealed good resolution (Figure 1F), and there was no clinical relapse at this writing.
Hemoptysis is most commonly caused by bacterial infections or fungi such as Aspergillus spp. Exophiala dermatitidis is a dematiaceous fungus that was described in a case of hemoptysis.(2) However, Cladosporium spp. apparently have yet to be reported as a cause of hemoptysis.
Cladosporium spp. are dematiaceous fungi which are found in a wide variety of habitats; they can be isolated from foods, such as peanuts.(3) They are saprophytic fungi, although they can cause human infections opportunistically; this genus has already been isolated from subcutaneous phaeohyphomycoses,(4) keratomycosis,(5) and from cerebrospinal fluid.(6) Specifically regarding the human respiratory tract, studies have re-ported Cladosporium spp. associated with hypersensitivity pneumonitis,(7) pulmonary fungus ball,(8) obstruction of the left main bronchus by a mucoid lesion,(9) and intrabronchial lesion.(10) Recently, C. cladosporioides was isolated from lung parenchyma.(1)
The pathogenic mechanism by which this fungus causes disease is still unclear. Apparently, fungus particles reach the lungs by inhalation, since C. cladosporioides is present in the microflora of peanuts.(3) It is possible that melanin, which is present in dematiaceous fungi, allows the maintenance of the fungus in lung tissue. It is a protective advantage against phagocytic cells during their oxidative burst.
Initially, we suspected of bacterial pneumonia, but previous antibiotic treatment had been administered without remission of clinical symp-toms. In addition, laboratory investigation of BAL fluid was negative for bacteria. However, Figure 1B shows an opacity with a ground-glass halo in a limited area of the right lung, compatible with pneumonia and alveolar hemorrhage. Therefore, based on clinical and radiological aspects, as well as positive cultures for C. cladosporioides from surgical biopsy fragments, we decided to start treatment with itraconazole, the drug of choice for the treatment of infections caused by dematiaceous fungi. (1,10) There was an excellent response to the treatment. Our findings rein-force the concern that Castro et al.(1) reported, which was that pulmonary phaeohyphomycosis is a challenge to the clinician and deserves atten-tion. It seems that infections of the respiratory tract due to Cladosporium spp. have been increasingly identified. The clinical manifestations are very similar to those of bacterial infections, and the clinician needs to differentiate between them, diagnose it, and treat it appropriately.
ACKNOWLEDGMENTSThis study received financial support from Fundação Araucária and from Brazilian Conselho Nacional de Desenvolvimento Científico e Tecno-lógico (CNPq, National Council for Scientific and Technological Development).
REFERENCES1. Castro AS, Oliveira A, Lopes V. Pulmonary phaeohyphomycosis: a challenge to the clinician. Eur Respir Rev. 2013; 22(128):187-8. http://dx.doi.org/10.1183/09059180.00007512
2. Barenfanger J, Ramirez F, Tewari RP, Eagleton L. Pulmonary phaeohyphomycosis in a patient with hemoptysis. Chest. 1989;95(5):1158-60. http://dx.doi.org/10.1378/chest.95.5.1158
3. Ismail MA. Deterioration and spoilage of peanuts and desiccated coconuts from two sub-Saharan tropical East African countries due to the associated mycobiota and their degradative enzymes. Mycopathologia. 2001;150(2):67-84. http://dx.doi.org/10.1023/A:1010863507652
4. Sang H, Zheng XE, Zhou WQ, He W, Lv GX, Shen YN, et al. A case of subcutaneous phaeohyphomycosis caused by Cladosporium cladosporioides and its treatment. Mycoses. 2012;55(2):195-7.
5. Chew FL, Subrayan V, Chong PP, Goh MC, Ng KP. Cladosporium cladosporioides keratomycosis: a case report. Jpn J Ophthalmol. 2009;53(6):657-9. http://dx.doi.org/10.1007/s10384-009-0722-3
6. Kantarcioglu AS, Yücel A, de Hoog GS. Case report. Isolation of Cladosporium cladosporioides from cerebrospinal fluid. Mycoses. 2002;45(11-12):500-3.
7. Chiba S, Okada S, Suzuki Y, Watanuki Z, Mitsuishi Y, Igusa R, et al. Cladosporium species-related hypersensitivity pneumonitis in household environments. Intern Med. 2009;48(5):363-7. http://dx.doi.org/10.2169/internalmedicine.48.1811
8. Kwon-Chung KJ, Schwartz IS, Rybak BJ. A pulmonary fungus ball produced by Cladosporium cladosporioides. Am J Clin Pathol. 1975;64(4):564-8. http://dx.doi.org/10.1093/ajcp/64.4.564
9. Feldman GJ. Mucoid lesion obstructing left main bronchus associated with isolation of Cladosporium fungal species. J Bronchol. 1999;6(3):183-5. http://dx.doi.org/10.1097/00128594-199907000-00009
10. YANO S, KOYABASHI K, KATO K. INTRABRONCHIAL LESION DUE TO CLADOSPORIUM SPHAEROSPERMUM IN A HEALTHY, NON-ASTHMATIC WOMAN. MYCOSES. 2003;46(8):348-50. HTTP://DX.DOI.ORG/10.1046/J.1439-0507.2003.00885.X